Veteran Suicide: A Growing Problem in Colorado
Veterans are disproportionately affected by suicide, especially those living in rural communities. In fact, a recent study showed that rural veterans have a 20 percent increased risk of suicide compared with veterans in urban areas.
Of the nearly 13,000 Coloradans who died by suicide between 2004 and 2017, nearly 2,600 were veterans. That’s nearly 200 veterans dying by suicide every year since 2004 in Colorado. Every number is a human life — someone’s loved one, dad, grandfather, mom, son, or sister.
Veterans and active-duty service members account for 20 percent of all suicides in Colorado, despite veterans only making up 9 percent of the state population. The suicide rate among veterans and active-duty service members in Colorado was more than two times higher than nonveteran adults in 2017, at 52.1 deaths per 100,000 compared with 22.1 per 100,000.
And it’s a growing tragedy. The rate of veterans dying by suicide per 100,000 has jumped since 2004, from 44.4 per 100,000 to 52.1 per 100,000 in 2017.
Colorado Veterans Die by Suicide Higher than National Rate
Colorado veterans are substantially more likely to die from suicide than other veterans across the country. The national rate in 2016 was 30.1 per 100,000, while the rate for Colorado that year is nearly double — 52.1 per 100,000.
Stigma, Not Availability, Blocks Mental Health Care for Veterans
To reduce veteran suicide, especially in rural Colorado, it is important to understand and address social, economic, and cultural factors unique to their communities. Veterans have different life experiences than people who have never served in the military, and data show they often are reluctant to seek mental health care.
The 2013 Colorado Health Access Survey (CHAS) — the most extensive survey in Colorado of health care coverage, access and utilization — offers some insight into mental health status and barriers to accessing mental health care for veterans.
Few Veterans Report Poor Mental Health in Colorado
Only 7.3 percent of veterans in Colorado report poor mental health, which the survey defines as experiencing eight or more days of poor mental health in the past month, compared with 12.3 percent of nonveterans in 2013.
These percentages may seem low, and they might reflect the difficulty of talking frankly about mental health. For some, it is an uncomfortable subject. People’s attitudes and beliefs about mental illness can lead them to deny symptoms, delay treatment, and suffer hardships. A national survey conducted by the U.S. Centers for Disease Control and Prevention (CDC) found that many people feel ashamed of their challenges or worry that others will not be sympathetic to their conditions.
Few Veterans Report Not Being Able to Access to Mental Health Care
Only 5 percent of veterans reported not being able to get mental health care they needed in the past year, significantly lower than the 9 percent of nonveterans. The true rate for both groups is likely larger. The CHAS data do not include people who didn’t want or admit to needing services.
Stigma is a Barrier to Veterans Accessing Mental Health Care
There are many reasons that someone might not get the care they need. The biggest difference between veterans and nonveterans is stigma.
The CHAS asked about two stigma-related reasons for not accessing mental health care — “You were concerned about what would happen if someone found out you had a problem,” and “You did not feel comfortable talking with a health professional about your personal problems.”
Nearly seven of 10 (69.3 percent) veterans in Colorado who said they did not get needed mental health care reported stigma-related reasons as a barrier. That’s nearly double the percentage of nonveterans (36.5 percent).
Veterans report other barriers to mental health care services — such as cost, believing insurance would not cover care, and difficulty getting an appointment — at similar percentages as nonveterans, suggesting these barriers to access are not unique to veterans. The biggest difference between veterans and nonveterans is the stigma they perceive when seeking care.
A Solution: A Suicide Prevention Pilot Program
While the rate of veteran suicide remains high in Colorado, the good news is suicide is preventable.
Many resources, programs, and organizations are addressing the problem. In fact, the U.S. Department of Veterans Affairs (VA) identified veteran suicide prevention as its top priority and has developed a National Strategy for Preventing Veteran Suicide, which emphasizes the need for more community-level initiatives and strategies.
Together With Veterans (TWV) is one such community-focused example in Colorado. It provides tailored suicide prevention training and equips rural communities with strategies to reduce stigma and promote help-seeking, with the ultimate goal of preventing suicide. Rural veterans are at higher risk of suicide than urban veterans, and are less likely to use mental health care than urban veterans.
The Together With Veterans model enlists rural veterans and their local partners, such as behavioral health providers, clinicians, and local leaders, to reduce suicide.
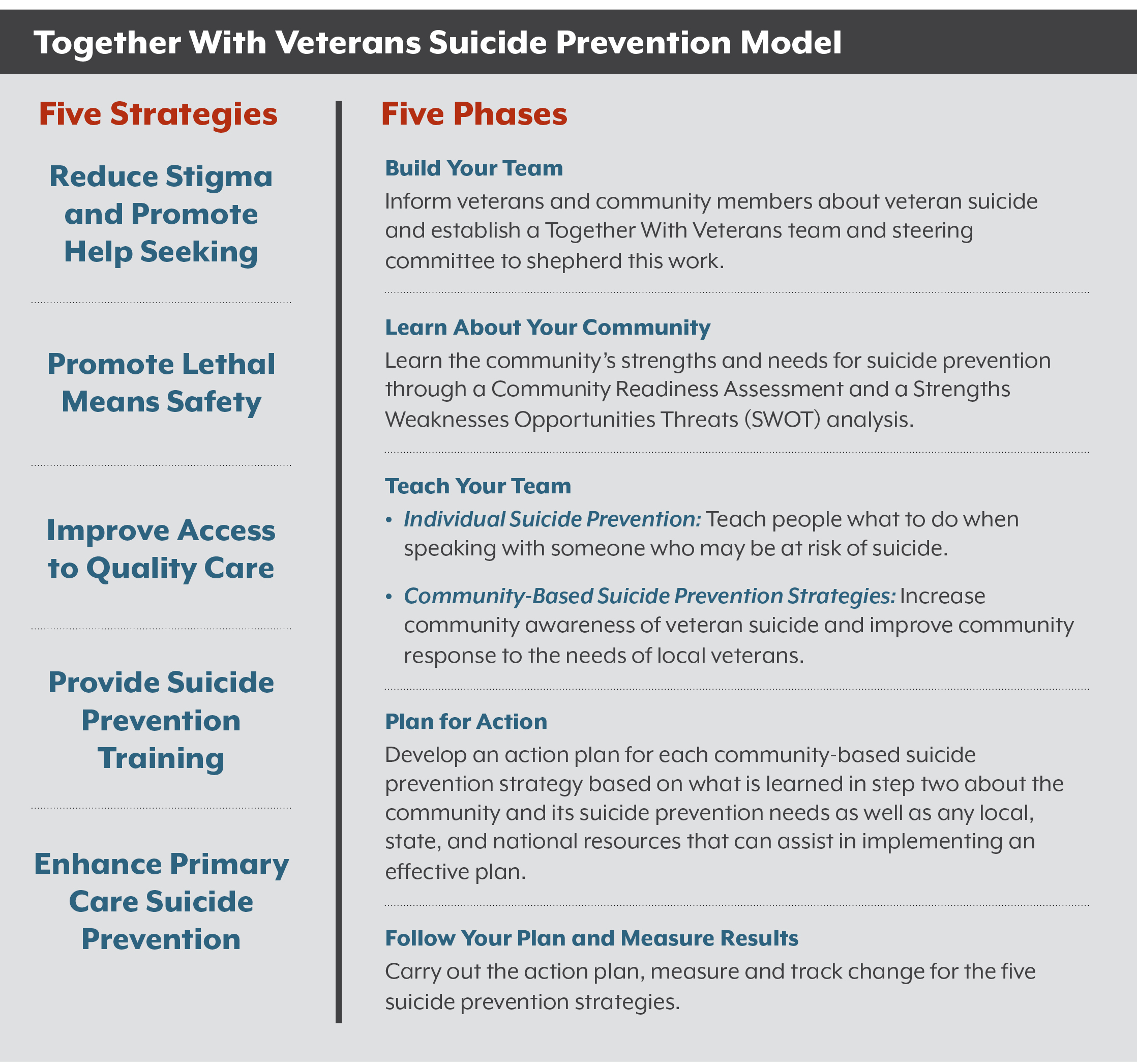
TWV uses five suicide prevention strategies to support local efforts (see box right).
These strategies are implemented using a five-phase process to guide communities in crafting a locally tailored plan. The process takes approximately a year and is continuously refined by the Together With Veterans team.
This model has been implemented in several rural veteran communities across the United States, including Colorado’s San Luis Valley.
In Alamosa, Conejos, Costilla, Mineral, Rio Grande, and Saguache counties, an organization called the Veterans Coalition of the San Luis Valley partnered with the Together With Veterans team starting in 2015 to implement the TWV model. The TWV team identified the San Luis Valley as an area with high suicide rates, so they worked with the Veterans Coalition to put together a locally tailored suicide prevention plan. The San Luis Valley plan includes a number of initiatives, including a veteran-to- farmer-program to ease the transition to civilian life, purpose-driven events to build a stronger community of veterans, and relationship-building efforts to connect behavioral health and primary care. Although the Veterans Coalition had been meeting for years, the TWV process gave the group a new level of credibility with veterans and other partners in the area and helped to develop a comprehensive action plan to focus their efforts.
The Veteran Health Connector
The success of the Together With Veterans work in the San Luis Valley attracted the attention of the Colorado State Innovation Model (SIM). Colorado SIM is a federally funded initiative focused on expanding access to integrated behavioral and physical health care, which included support for Regional Health Connectors (RHCs) and local suicide prevention efforts across the state. RHCs are a new workforce to improve the coordination of local services to advance health in communities in Colorado. In the San Luis Valley, the local RHC helped link the Veterans Coalition to health care resources and transportation services in the region, much needed by veterans in that area. Thanks to this connection, the Veterans Coalition is now developing a transition program to hire veterans as drivers for a new transportation service in the area.
Leveraging the strengths of both the RHC and TWV models, SIM partnered with the VA to replicate this work in northeast Colorado by creating the Veteran Health Connector (VHC) position, a full-time role to coordinate local efforts to prevent veteran suicide using the Together With Veterans model. The initial intent of the work was to connect veterans with existing community resources to help ensure their health and wellness, and specifically address suicide risk. The position is hosted by the Centennial Area Health Education Center (CAHEC) in Greeley, Colorado, and the VHC’s work spans northeast Colorado. This region includes Logan, Morgan, Sedgwick, Phillips, Washington, and Yuma counties and is home to over 4,500 veterans. From 2004 to 2017, nearly 30 veterans in this region died by suicide, underscoring the need for preventative action.
The Veteran Health Connector, Stacy Syphers, a veteran from Morgan County, has been forming a community coalition focused on suicide prevention for veterans in northeast Colorado.
Veteran Health Connector Profile: Stacy Syphers
On the twenty-second day of each month, about 20 people gather near the town center of Brush, about 90 miles northeast of Denver. They are veterans, business leaders, and other community members, and they hold signs that explain why they are there: “Did you know? 22 Veterans Every Day Commit Suicide.” “22 is too many.” “Veterans Crisis Line: 1-800-273-8255.”
Stacy Syphers, a veteran who lives in the Brush area with her family, has been working to change that as a Veteran Health Connector, read her story.
Two Phases Down, Three to Go
From January through June 2019, Syphers guided the first two of the five phases of the TWV process in the Morgan County community of Brush. This work has been in coordination with the Together With Veterans Team at the VA Rocky Mountain Mental Illness Research, Education and Clinical Center (MIRECC), Western Interstate Commission for Higher Education Behavioral Health Program (WICHE BHP), the VA Center of Innovation (COIN), Centennial Area Health Education Center (CAHEC), and the Colorado Health Institute (CHI).
In the first phase, Syphers helped build a team of local veterans, community leaders, and providers to drive the Together With Veterans work forward. She assembled the Steering Committee, responsible for shepherding the program, and working with the Together With Veterans staff at the MIRECC and WICHE BHP to identify needs for their community in veteran suicide prevention.
To better understand the community’s needs in Brush, the team moved to the second phase, which included a Community Readiness Assessment and a SWOT analysis. The Community Readiness Assessment involved a focus group of community members that helped determine local awareness, attitudes, and commitment to addressing veteran suicide prevention. Syphers identified members of the community to participate in the focus group and conducted the Community Readiness Assessment with assistance from the team at MIRECC.
Soon after, Syphers organized a SWOT analysis, with help from WICHE, to guide the TWV Steering Committee to identify strengths and opportunities that are helpful in addressing veteran suicide, and weaknesses and threats that create barriers to implementing a community-based suicide prevention action plan.
Next Steps for TWV and Veteran Suicide Prevention on the Eastern Plains
Phase Three of the five-phase process is set to begin this summer. Members of the Brush TWV team will learn suicide prevention strategies, which will lead into a comprehensive action plan tailored to, for, and by veterans on the Eastern Plains.
While short-term funding for the VHC and TWV process catalyzed this work in Brush, the goal of the TWV process is to create a locally tailored suicide prevention plan, which will likely require long-term funding. Over the next year, the Steering Committee will need to factor in long-term sustainability when selecting strategies to include in the suicide prevention action plan.
The Mission Continues
Programs like the Veteran Health Connector and prevention models like Together With Veterans are empowering communities with veteran-driven suicide prevention strategies that bring all players into the fold with the goal of saving lives. These programs help build community awareness and offer tangible opportunities for families, friends, and neighbors to support one another. Community awareness and supportive actions can help to address stigma — veterans’ biggest barrier to receiving mental health care when they need it. While changes in attitudes and culture happen slowly — over years, if not decades — community-led initiatives are leading the way toward a brighter future for all veterans.
Full endnotes for this research are available in the PDF version of the report.