COVID-19 cases are on the rise nationwide now that most states have opened up. Colorado noticed an increase in cases last week after steady drops since late April, but generally, things are still looking up — and trending down.
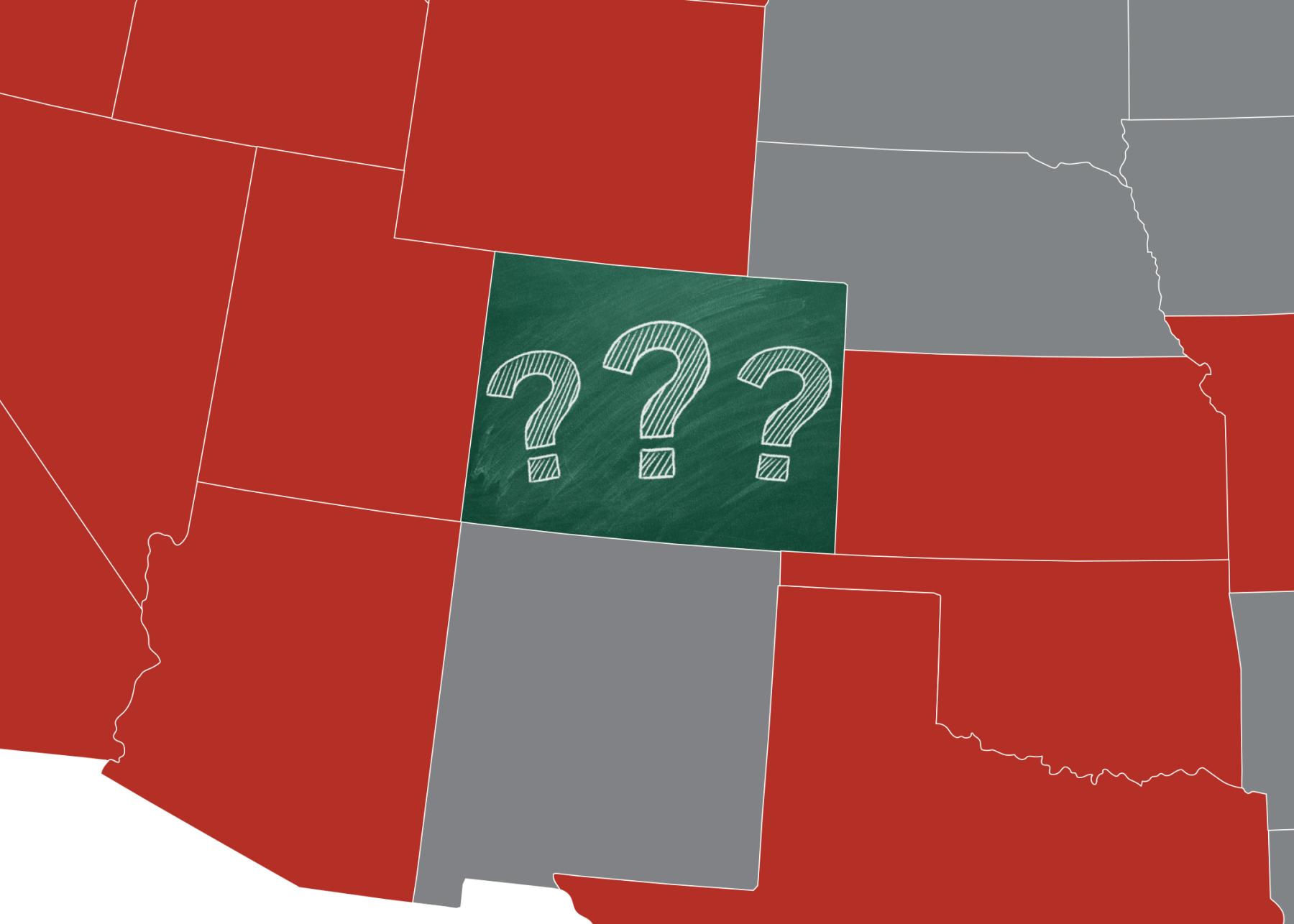
This has many wondering: What makes Colorado different? This week, the Colorado Health Institute puts a few theories to the test and takes a look at why it matters as we move into summer and fall.
Theory: Colorado is a younger state, so we are at a lower risk than other parts of the country.
Colorado is a relatively young state, with a median age of 37.3, compared to 41.6 in Florida, one of the states worst hit by recent outbreaks. But other hard-hit states have similar age demographics — for example, Arizona, with a median age of 37.1, now has the highest rate of new infections in the country.
And while younger people are less likely to be hospitalized due to COVID-19, they are not invincible and still play a key role in transmission. So, while our age isn’t hurting us, it’s likely not the explanation here.
Looking forward: How might age affect the epidemiological curve this summer?
Recent data warn of a concerning trend for a younger state. The number of new cases among Coloradans under age 30 is on the rise, making up around 40% of the state’s COVID-19 cases.
This may be due to more widespread testing that is identifying mild infections, which are more likely to be found in younger people. If this is the case, we can expect an increase in reported cases across all age groups but little change in hospitalizations.
It’s also possible that older adults are being more cautious, causing them to make up a smaller percentage of new cases. The state has successfully reduced outbreaks in nursing home facilities. In this case, we can expect a drop in the number of new cases among older people and a decline in hospitalizations.
More worrisome, a third explanation is that young people are becoming less cautious as the state opens up restaurants and bars. In Boulder, Eagle, and San Miguel counties, the virus has been spreading rapidly among younger adults gathering in large groups. In this case, we can expect the number of new cases to rise among young people and more young people to be hospitalized.
While around 40% of positive cases are asymptomatic, this percentage is closer to 50% for younger people. This means that as we move forward, it is even more important for younger adults to practice harm reduction: wearing masks, washing hands, limiting outings, and avoiding large gatherings.
Theory: Colorado is relatively a healthier state, meaning fewer people are being hospitalized and outcomes are better.
Indeed, Colorado has lower rates of chronic conditions than other states. Our geography helps with that by providing accessible outdoor recreation. Colorado’s population is whiter and wealthier than the national average, and race and income correlate strongly with health outcomes.
Through the course of this pandemic, Coloradans have continued to find ways to stay active, and the state has helped with promoting social distancing, such as closing some streets to allow for cyclists, runners, and dog-walkers to be more than six feet apart. But it’s incorrect to think that Colorado is home to only fit, outdoorsy people. Many of us battle chronic diseases, live in cities with poor air quality, and lack access to outdoor recreation.
Looking forward: Are disproportionately impacted Coloradans getting lost in the data?
Many people cannot be “safer in the vast, great outdoors” for a variety of reasons. While our relative health is a protective factor, many Coloradans are at higher risk for COVID-19 because they are people of color, earn low incomes, or are experiencing homelessness. It is critical for the data to shine a spotlight on these people to ensure we are doing enough to protect them.
There is good news though. Hospitals are getting better at treating people who still become gravely ill.
Seven hospital systems that have treated 96% of the hospitalized COVID-19 patients in Colorado released new data this week that demonstrate how hospitalization trends look different from the spring.
Hospital mortality rates dropped significantly over time, from over 15% in March and April to 10.5% in May. The average length of stay also fell from about 12 days in March to seven days in May.
And Colorado hospitals are being more conservative about putting patients on a ventilator. Ventilator rates dropped from 29% in March to 13% in May. This is important because outcomes were worse for patients who needed ventilators. As fewer people are needing them, Coloradans can hopefully expect outcomes to be better.
As health care workers continue to gain new knowledge on how to care for patients, data and provider practices show some promising results.
Theory: Our approach was strong.
Colorado enacted strict public health interventions, including a mandatory stay-at-home order and strong encouragement for masks, earlier than most states. The state was one of the first in the country to put this order in place — encouraging people to stay home, limit gatherings, and work from home if possible. And Coloradans rose to the challenge. Significant numbers of us limited our interactions with others and quickly embraced mask-wearing.
There is no denying that the closing of non-essential businesses harmed the state’s economy and forced many Coloradans out of work. But in hindsight, the statewide approach appears to have curbed the spread of the virus at a critical time.
Looking Forward: How will the new “Protect Our Neighbors” order work?
The phase two, Safer-At-Home, order was modified on June 1 and since then, non-essential businesses — including restaurants, bars, gyms, and workspaces — have started reopening. Cities and counties soon could start moving into the next phase, Protect Our Neighbors, which relaxes even more restrictions. We can expect some new transmissions as a result.
Recent data from the Colorado Department of Public Health and Environment show that as of June 24, there have been 4,600 confirmed or suspected COVID-19 cases from outbreaks in workplaces across the state — more than in nursing homes.
This makes sense. Most workplaces were closed during earlier stages of the pandemic and are now navigating how to comply with public health interventions.
Mobility data show that Coloradans are spending more time in public, too. Colorado can expect cases and outbreaks at more frequent rates in places that are now open, but the good news is that the lockdown gave the state time to implement contact tracing, organize temperature checks, and normalize mask-wearing.
What Should We Expect from the Summer?
Our state is seeing positive impacts of some of our protective factors, but we are not in the clear. As Denver Mayor Hancock said Wednesday morning, we are still in the first quarter of a football game.
It’s crucial to learn more about why Colorado’s numbers look better than our neighboring states, highlight people who the data might mask, and continue evaluating what our secret may be. We must also entertain the possibility that we’ve just been lucky.
Whatever we’re doing right, we need to keep doing it as we go into the second weekend of summer and approach the Fourth of July holiday.
Related Blogs and Research