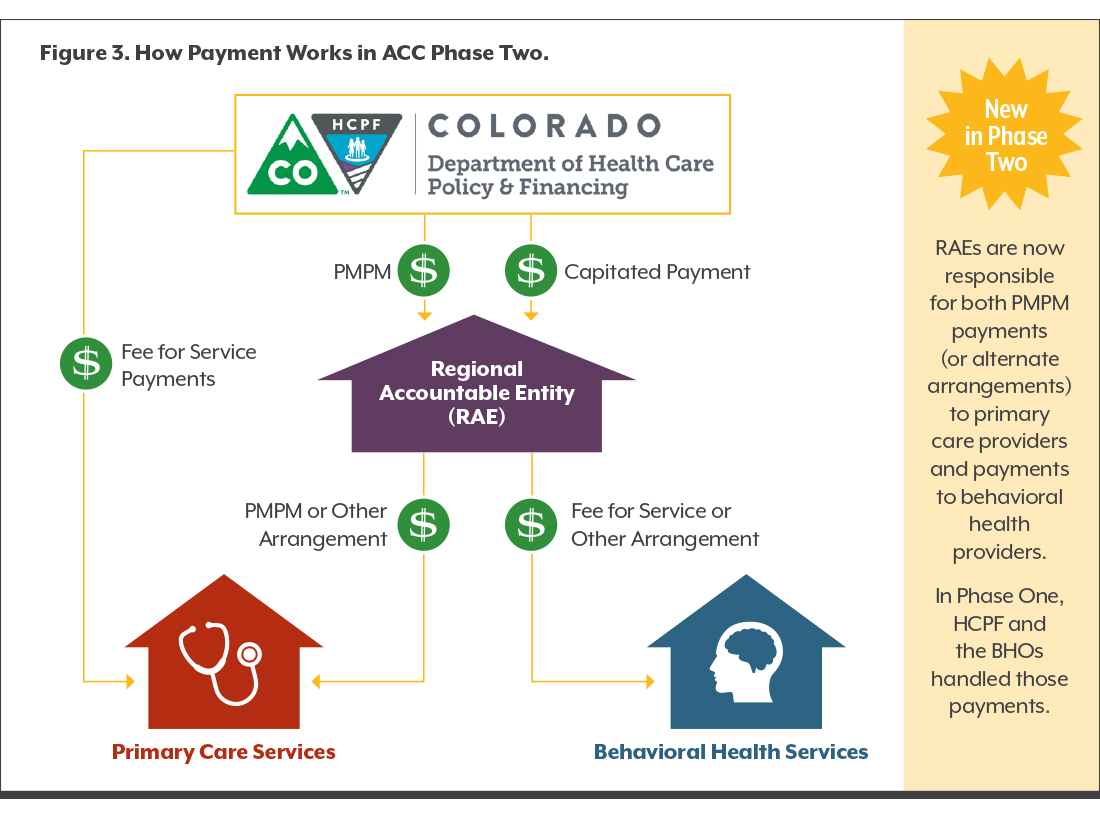
What is the Role of RAEs in Paying Providers?
Payment is often used as a tool to shift provider behavior and bring about system-wide change. RAEs play a larger role in paying providers than their predecessors, the RCCOs.
The graphic on the right shows how these four types of payment flow from HCPF to primary care and behavioral health providers in the ACC’s Phase Two. The key takeaway from the graphic that one entity — the RAE — is now responsible for both the PMPM payment (or alternate arrangement) to primary care providers and payments to behavioral health providers. In Phase One, HCPF and the BHOs handled those payments.
Some payments have not changed since Phase One. Primary care providers are paid on a fee-for-service basis, and behavioral health services are paid on a capitated rate. Extra incentive payments aim to push the ACC’s big idea — that focusing on improving the health and experience of Health First Colorado members saves the state money in the long run.
But Phase Two makes some important changes in the way money flows:
- The RAE passes along incentive payments to primary care providers (although HCPF still pays primary care providers for medical services to Health First Colorado members). The RAE also handles all payments to behavioral health providers.
- In Phase One, HCPF paid incentives to providers based on how the provider’s entire RCCO region performed on a set of metrics called the Key Performance Indicators (KPIs). For example, one KPI measured Medicaid members’ use of the emergency department. In Phase Two’s first year, HCPF increased the number of KPIs from three to seven, with the possibility of expanding the number of indicators in the future. Similar to Phase One, the KPI payment from HCPF to the RAE is based on the overall regional performance of the RAE. The difference in Phase Two is that RAEs — and not HCPF — make the KPI payments to primary care providers.
- Phase Two introduces additional opportunities for RAEs and providers to earn incentive money for improving the quality of care. Primary care providers contract directly with RAEs in Phase Two, which gives RAEs more latitude than RCCOs had to develop innovative payment approaches with providers. The question remains as to whether these incentives will improve health and save money for the state.
What are the Big Questions Heading into Phase Two?
As Phase Two of the ACC unfolds, CHI is monitoring a few key questions:
How will changes in attribution affect members and providers? HCPF’s changes to its attribution approach are intended to make life easier for primary care providers by ensuring that they will only have to contract with a single RAE. The changes are also intended to preserve members’ choice of providers while linking them to the primary care provider with whom they’ve had a prior history as a medical home. Yet the complicated exercise of linking over a million members to thousands of providers raises many questions, especially because attribution determines the volume of PMPM payments that RAEs receive. Will HCPF attribute the expected number of members to each provider? What happens if providers aren’t assigned all the patients they are expecting? And how will attribution handle exceptions, like when a chronic care patient’s main care provider is a specialist instead of a primary care clinician?
How will changes in the way care is paid for in Medicaid impact cost, quality and access to care? The ACC counts improving Health First Colorado members’ access to care and quality of care — as well as saving Medicaid dollars — among its key objectives. There are a few promising areas where this could happen in Phase Two. First, RAEs can develop innovative arrangements with primary care providers that encourage efficiency and quality. Second, Phase Two continues the emphasis on coordinating care — potentially avoiding duplicative services and ensuring patients get the right care at the right time. Finally, Phase Two places an even greater emphasis than Phase One did on tracking progress through data and measurement, then tying improvement to financial incentives. HCPF, RAEs and providers are figuring out ways to make the data they need available in a timely fashion. Understanding the ways in which RAEs and providers are using these tools will be key to evaluating Phase Two’s success.
How will success be measured? The many elements of the ACC mean that success can be measured in many ways. Cost savings to the state is one; performance on key metrics is another. Phase One included an evaluation of cost, quality and utilization in the ACC conducted by the University of Colorado Denver.4 Are there plans to evaluate Phase Two, and what can be learned about each RAE’s strategies, successes and challenges?
Phase Two includes the added dimension of public reporting of data. HCPF aims to increase transparency and focus on improving the health of populations by posting a dashboard of metrics. This dashboard includes KPIs and additional clinical and public health measures, such as suicide rates, developmental screening and medication management of asthma.
How will the six behavioral health visits primary care providers can now bill for and other Phase Two changes affect access to behavioral health services? Phase Two includes several ways to improve access to behavioral health services. For example, primary care provider practices or clinics are now allowed to bill for up to six short-term visits to a Medicaid-enrolled, licensed behavioral health clinician in a primary care setting.
Each RAE also has to develop a statewide network of behavioral health providers. Previously, BHOs reviewed behavioral health providers and allowed those it approved to bill for services. The process is called credentialing. Many smaller or independent providers felt shut out of Health First Colorado because they could not get credentialed. Now RAEs are in charge of credentialing in their regions. Some behavioral health providers may have to contract with multiple RAEs in order to serve patients with primary care providers in different regions. Will the RAEs’ new systems increase the number of behavioral health providers in their networks, and will these changes improve access to behavioral health care or oversaturate the market?
How will RAEs manage the integration of physical and behavioral health? Behavioral health in Health First Colorado is a capitated managed care program. While each RAE either has experience managing behavioral health care or has a managed care organization as a partner, there will still likely be a learning curve for some of them in administering payments, working with providers and providing care coordination services. How will patient care be affected by having one organization manage both primary care and behavioral health care services for the member? How will two very different payment systems — fee-for-service and capitation — work together under the same roof?
How will RAEs collaborate with providers in the health neighborhood? In Phase Two, RAEs may contract not only with primary care and behavioral health providers, but with other providers in their “health neighborhood,” including dentists, specialty care providers, local public health agencies and hospitals. These relationships hold the potential for RAEs and their partners to implement innovative approaches that address challenges with Health First Colorado members’ access to services. They also may be given lower priority as RAEs work within their budgets to ensure access to primary care and behavioral health first.
Who will be at the table to inform RAEs’ strategic direction? Each RAE is supposed to solicit ideas from stakeholders to inform their strategy. Consumer and provider representation is of particular interest. How will the perspective of Health First Colorado members be considered? And to what extent will the perspectives of providers of all types and sizes be included?
Conclusion
With the launch of Phase Two, the Accountable Care Collaborative is now the primary way Colorado’s Medicaid program is aiming to cut costs and improve care for more than one million Medicaid members.
Phase Two also marks the state’s most tangible step yet in its goal of integrating primary care and behavioral health. By putting one entity in charge of arranging both physical and mental health care for Health First Colorado members, the ACC’s architects hope that care will become more integrated not just in the clinic, but also behind the scenes.
The overarching question is whether changes in Phase Two will maintain or increase access, reduce costs and improve care. Phase Two places a lot of faith in private organizations that own Regional Accountable Entities to understand local needs and encourage better care for a lower price.
The future of the state’s Medicaid program rests in large part on how this vision unfolds.