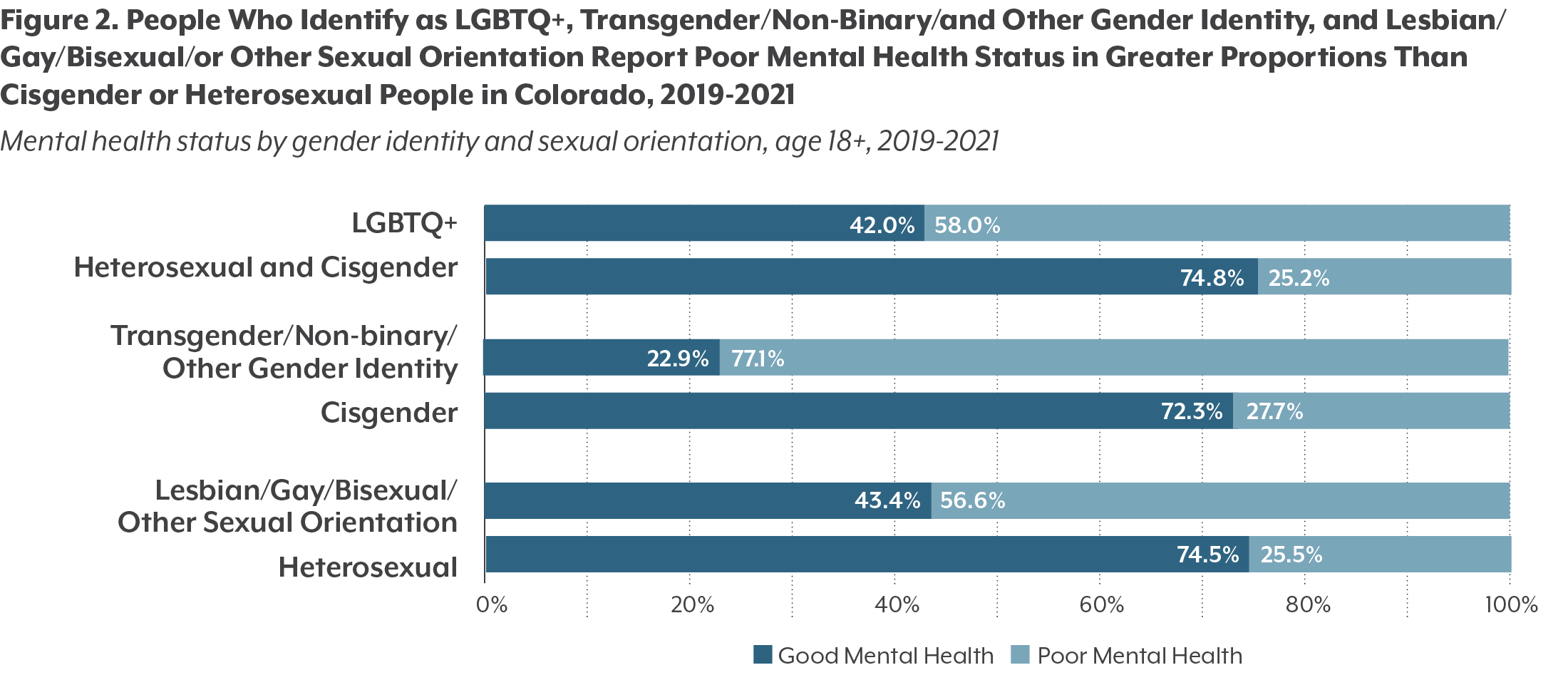
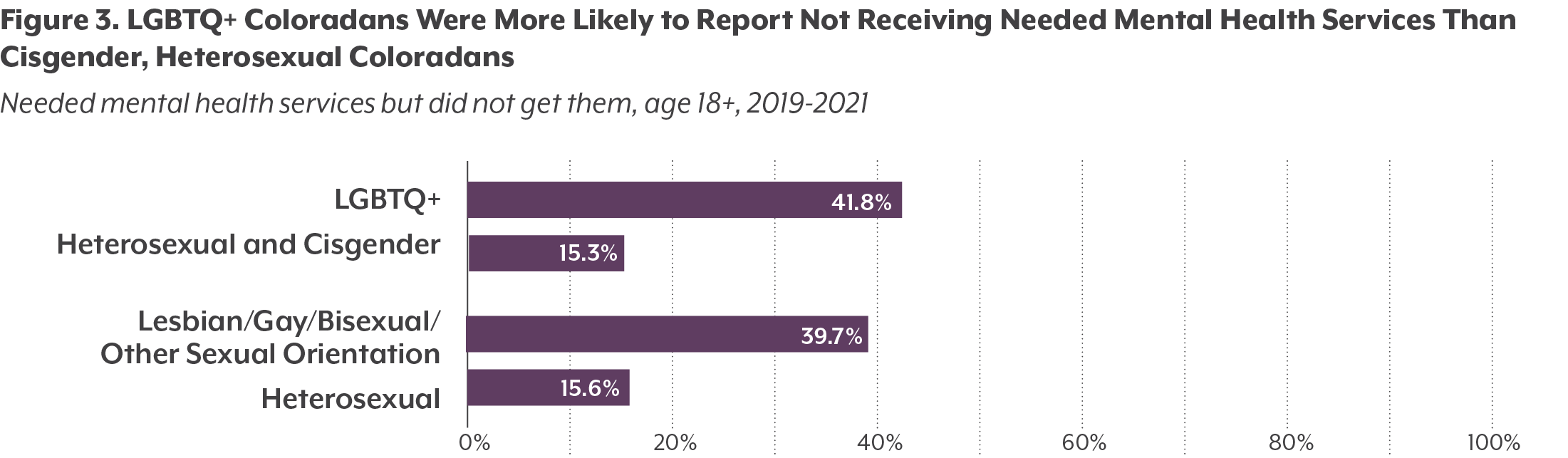
Poor mental health is common among LGBTQ+ people across the United States. They are 2.5 times more likely to experience depression, stress, and substance misuse. About four in 10 adults in the U.S. transgender population have attempted suicide in their lifetime. Worse mental health outcomes, including increased prevalence of substance use and misuse, among LGBTQ+ Americans is likely due to lack of social support and community acceptance, socioeconomic challenges, and lack of access to LGBTQ-competent services. A rise in crime against LGBTQ+ individuals, as well as increased presence of anti-LGBTQ groups, may also contribute. 2021 also saw a greater number of anti-LGBTQ bills passed across the nation than any year previously.
Colorado has some of the country’s strongest legal and policy protections for LGBTQ+ individuals, according to a 2020 report by the Human Rights Campaign, an LGBTQ-advocacy organization. But there is an opportunity to fortify social supports and improve access to mental and behavioral health services. CHI combined data from the 2019 and 2021 Colorado Health Access Surveys (CHAS) and found that LGBTQ+ Coloradans were much more likely to report feelings of depression or stress than Coloradans who are heterosexual or cisgender — a term for those who identify with the gender they were assigned at birth.
Methodology
CHI combined responses of people identifying as lesbian, gay, bisexual, transgender, or queer into a single category (LGBTQ+) for analysis. The “Q+” is intended to include people identifying different orientations and all non-male or non-female gender identities other than lesbian, gay, bisexual, and transgender identity.
The CHAS questionnaire only asked respondents ages 18 and older about their sexual orientation and gender identities. As a result, this report only provides information about the mental health of adult Coloradans.
In some cases, data from 2019 and 2021 were combined to provide a reliable sample size. Survey years 2019 and 2021 were combined to create a large enough sample size to report on specific gender and sexual orientation identities on the CHAS. Weights were then applied to the sample to create estimates that reflect an average of the two years for the adult respondent population.
A Largely Urban Population
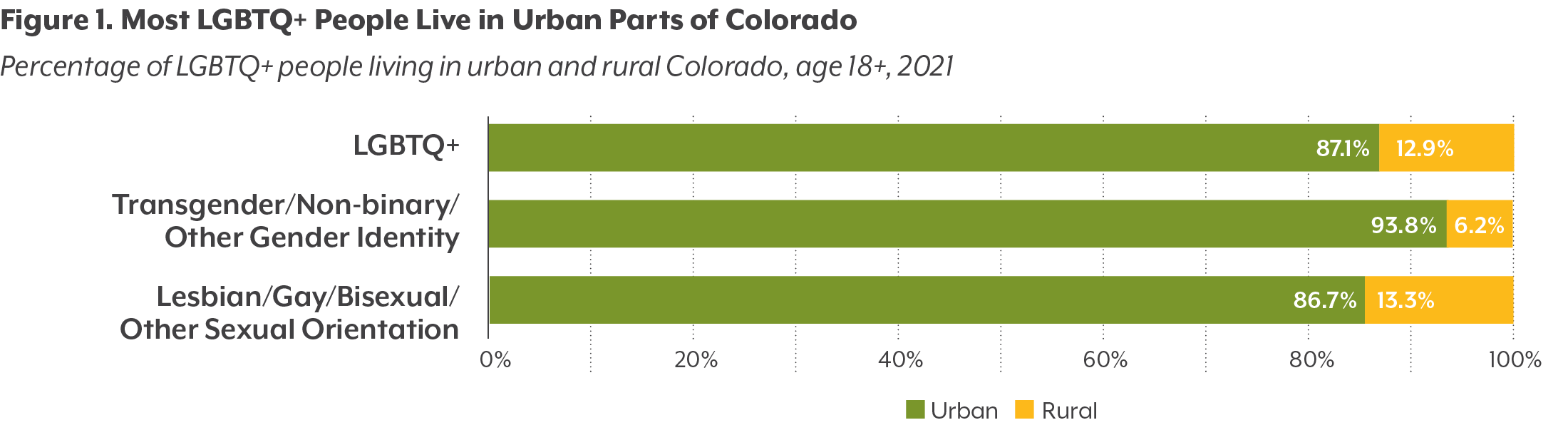
According to the 2021 CHAS, about 7.8% of Coloradans 18 years of age or older identified as LGBTQ+. This estimate is slightly higher than recent national estimates, a discrepancy that is likely primarily due to differences in methods. Colorado’s LGBTQ+ population includes the 7.3% of Colorado adults who identified as lesbian, gay, bisexual, or another non-heterosexual sexual orientation, and 1.2% of Coloradans who identified as transgender, non-binary, or otherwise gender diverse.
CHAS data from 2019 and 2021 indicate that the majority (87.1%) of Colorado’s LGBTQ+ population lived in urban areas, compared to 82.0% of all Coloradans. (See Figure 1.) Data for other demographic breakdowns, including race and ethnicity data, were not large enough to provide reliable data.