These inequities have resulted from historical exclusion and racism that continues to pervade our education, criminal, housing, and health care systems. Experts anticipate increased mental health needs in the wake of COVID-19, which heightens the need to address stigma and systemic barriers that create disproportionate access to mental health care for people of color.
Mental health stigma is a persistent challenge for many. Nearly half (47.3%) of Coloradans who said they did not get needed mental health care cited stigma as a reason in 2019. There are countless reasons a person can be reluctant to seek care, but for people of color, cultural factors can make the stigma around mental health especially difficult to overcome.
While the experiences of different racial and ethnic groups and individuals are unique, some harmful notions about mental health can be magnified for people of color. These mental health myths create additional hurdles to seeking care.
- Myth: A mental health condition is nothing compared with the hardships experienced by previous generations.
- Myth: A mental health condition is a sign of weakness.
- Myth: A mental health condition is shameful.
Compounding mental health stigma is the system of oppression that exists from centuries of racism and discrimination.
Systemic barriers prevent people of color from accessing care and treatment.
For as long as the U.S. has existed, people of color have faced race-based exclusion from accessing health, educational, social, and economic resources. Today, disparities persist and are reflected in lower rates of health care access and treatment.
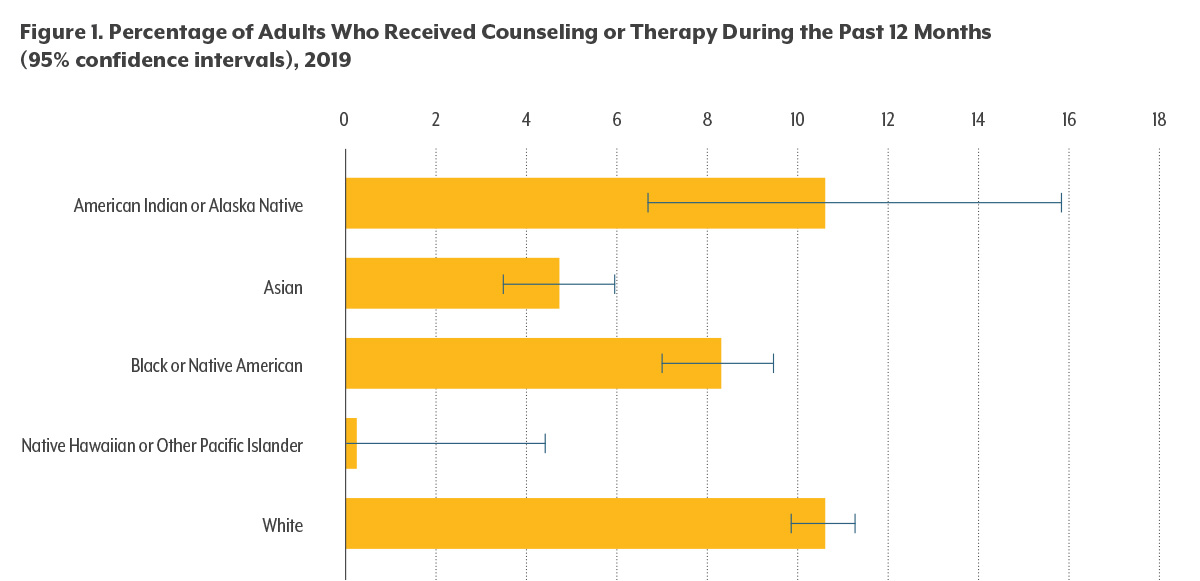
Data from the Centers for Disease Control and Prevention (CDC) show that white adults were significantly more likely to have received mental health counseling in the past 12 months than Black or African American, Asian, or Native Hawaiian/Pacific Islander adults (see Figure 1).
Good health is not equally distributed, and systemic problems continue to negatively impact health outcomes for people of color.