In December, after months of anticipation, Colorado received its first shipment of COVID-19 vaccines. With it came hope that the end of the pandemic might be within reach — and a slew of complex questions about whom to prioritize for early vaccines.

The Pandemic Behind Bars
Colorado’s vaccine distribution plan does not prioritize people who are incarcerated or detained. But new analysis from the Colorado Health Institute (CHI) shows that COVID-19 has spread through Colorado’s prisons, jails, and other correctional and detention facilities at an alarming rate.
Outbreaks at prisons, jails, and other correctional and detention facilities account for 1 in every 24 cases of COVID-19 in Colorado since the start of the pandemic, and 15 of the 20 largest outbreaks in the state have occurred in prisons and jails.
Please note that CHI’s analysis is based in large part on COVID-19 outbreak data published by the Colorado Department of Public Health and Environment (CDPHE) on January 20, 2021, and COVID-19 case data published by the Federal Bureau of Prisons on January 22, 2021. Unless otherwise noted, it does not include additional data on COVID-19 cases collected by other entities, nor does it capture changes in case numbers since the dates noted above. More information on sources is available at the end of this report.
Colorado’s Vaccine Distribution Plan
In accordance with federal guidance, Colorado’s vaccine distribution plan begins with health care workers who work closely with COVID-19 patients, as well as staff and residents of long-term care facilities such as nursing homes and assisted living facilities, where the spread of the virus has been particularly devastating. Next, in what the state calls “Phase 1B,” are Coloradans 70 and older, other health care workers, and first responders, followed by frontline essential workers, essential government officials, and frontline journalists. Phase 2 includes people ages 60-69, people with medical conditions that put them at higher risk, other essential workers and government officials, and adults who received a placebo during a COVID-19 vaccine clinical trial. Last, in Phase 3, is the general public — people over 16 not identified in any of the earlier priority groups.
But the state’s vaccine distribution plan has not always looked this way.
A previous version of the plan, shared by the state in October, included a priority population no longer mentioned in the current plan: people who are incarcerated.
Previously, people in “congregate housing,” including incarcerated people, were placed at the beginning of Phase 2, after Colorado’s “critical workforce” and residents of long-term care facilities, but ahead of older adults, people with medical conditions, and the general public.
But after a guest editorial in The Denver Post blasted Gov. Jared Polis for prioritizing incarcerated people over older adults, the governor pivoted. At a press conference two days later, in early December, a reporter asked Polis about the prioritization of incarcerated people, referencing the editorial specifically. Polis replied, “There’s no way [the vaccine is] going to go to prisoners before it goes to the people who haven’t committed any crime,” adding that the proposed distribution plan would be amended. His office later clarified that “inmate status will not make a difference in terms of timing of receipt of the vaccine,” and that inmates who fell into a priority group, such as people over 70 or people with a high-risk medical condition, would be eligible to receive the vaccine at the same time as others in that category.
Colorado’s vaccine distribution plan has since been adjusted. Under the revised plan, people who work in correctional facilities are slated to receive their vaccines as part of Phase 1B, just as they were before. Any mention of the people held in those correctional facilities, however, has disappeared from the list altogether.
The Spread of COVID-19 in Colorado’s Correctional and Detention Systems
The spread of COVID-19 through Colorado’s correctional and detention facilities has been both profound and far-reaching, according to COVID-19 outbreak data published by the Colorado Department of Public Health and Environment (CDPHE) (supplemented here by data from the Federal Bureau of Prisons).
Since the start of the pandemic, over 16,000 cases have been reported at Colorado prisons, jails, or other correctional and detention facilities.
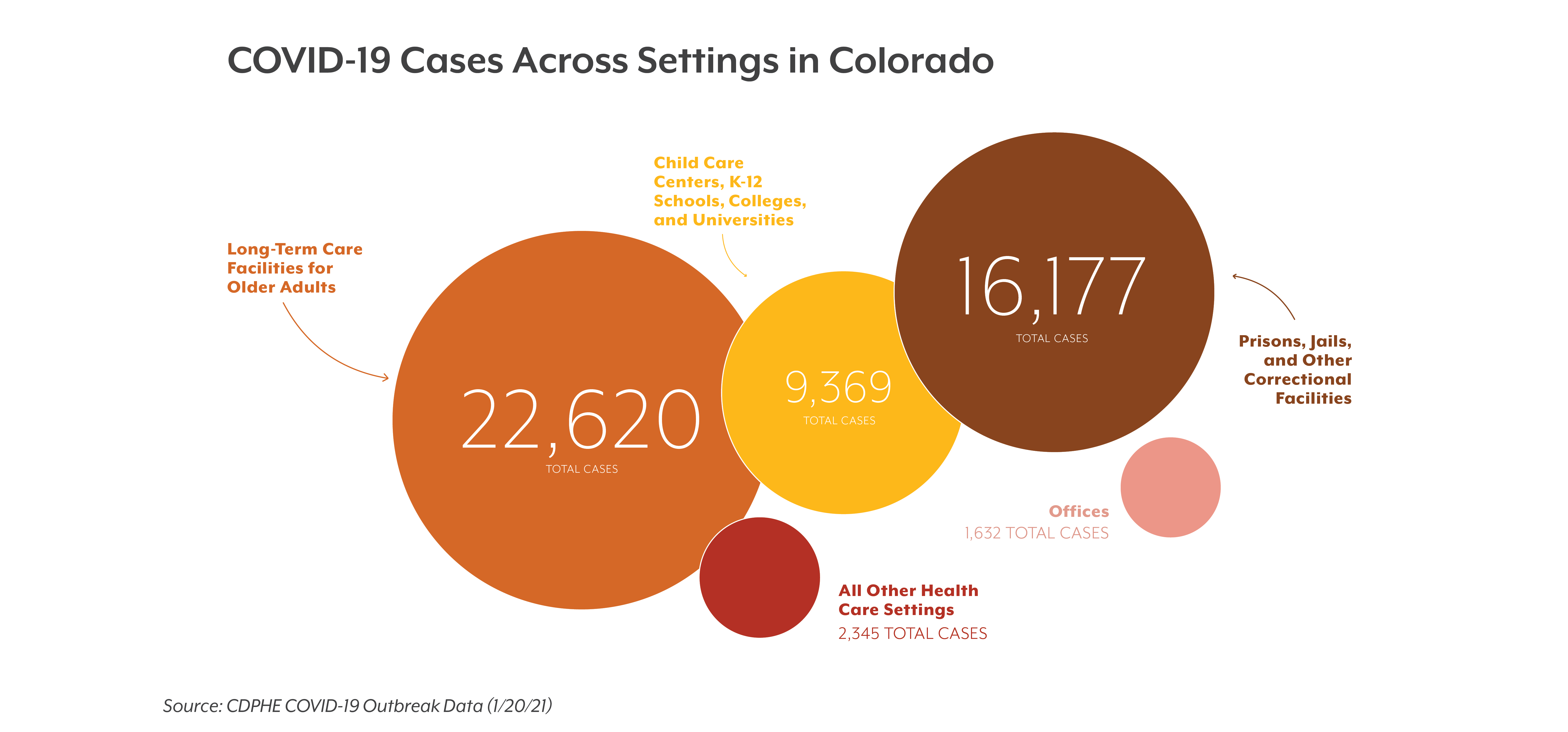
For comparison, that’s about 6,000 fewer cases than have been reported at long-term care facilities for older adults (22,620). It’s also more than the number of cases reported in other health care settings (2,345); child care centers, schools, colleges, and universities (9,369); and office spaces (1,632) combined. (See figure below.)
Vaccination plans have prioritized older adults and people with underlying health conditions because they are more vulnerable to severe illness, and mortality rates in long-term care facilities and other health care settings are extraordinarily high — higher than in prisons and jails. But national studies indicate that mortality rates among incarcerated people are significantly higher than those of the general public. And regardless of the circumstances leading up to one’s incarceration or detention, exposure to a life-threatening illness (with the potential for long-term health effects) is not part of their prison sentence or terms of detention.
By the Numbers: COVID-19 in Colorado Correctional and Detention Facilities
16,177 cases and 32 deaths have been reported at Colorado correctional and detention facilities.
1 in every 24 cases in Colorado has been part of an outbreak at a correctional or detention facility.
15 of the 20 largest outbreaks in the state have occurred in prisons and jails.
For every 1,000 people incarcerated in Colorado prisons, 557 prisoners have contracted COVID-19.
20 out of 21 state prisons,
4 out of 4 federal prison facilities,
19 jails, and
the state’s ICE detention facility have reported outbreaks.
An additional 52 outbreaks have been reported at other types of correctional facilities, such as community corrections centers and residential treatment centers for justice-involved people with substance use disorders.
This is a national problem. The Marshall Project estimates that one in five people incarcerated in state and federal prisons in the United States has tested positive — a rate four times higher than the general population.
According to the Centers for Disease Control and Prevention (CDC), outbreaks in settings such as prisons and jails are uniquely difficult to control due to “the inability to physically distance, limited space for isolation or quarantine, and limited testing and personal protective equipment resources.”
The CDC also notes that people in correctional and detention facilities “may also be older or have high-risk medical conditions that place them at higher risk of experiencing severe COVID-19.” According to the Colorado Department of Corrections, 30% of people incarcerated in Colorado state prisons have “medical needs,” 35% have “mental health needs,” and 7% are over 60.
COVID-19 in correctional and detention facilities also presents a threat to the general public. Correctional staff, attorneys, and medical providers who work in these settings not only risk carrying the virus into their place of work, they also risk bringing the virus home to their families and the greater community. Additionally, inmates and detainees have limited ability to quarantine before release, which can further contribute to the transmission of COVID-19 into the surrounding community. Jail and prison walls are permeable — hundreds of people are released from Colorado jails and prisons every day. As a result, outbreaks inside these facilities contribute to outbreaks in the greater community — and vice versa.
Given these challenges, the CDC recommends vaccinating incarcerated and detained people at the same time as correctional staff.
Of the 16,177 cases reported at Colorado correctional and detention facilities, 2,330 have been among staff and 13,827 have been among people who are incarcerated, detained, or otherwise residing in correctional settings.
In total, there have been 32 recorded deaths. Of the 32 people who died, 31 were considered “residents” of a correctional or detention facility.
COVID-19 has spread to nearly every corner of the state’s detention and corrections apparatus, including state prisons, federal prisons, the U.S. Immigration and Customs Enforcement (ICE) detention facility in Aurora, and city and county jails.
The extent of the spread in each of these settings is described in further detail below.
State and Federal Prisons
There are 21 state prisons in Colorado (19 state-run prisons and two private prisons). As of this month, 20 of the 21 state prisons have reported outbreaks. The only prison that has not reported any cases of COVID-19 is the smallest in the state — Colorado Correctional Center in Golden houses 81 inmates.
Colorado is also home to two federal prison complexes, one in Englewood and one in Florence. They collectively span four federal prison facilities — all four of which have reported outbreaks.
In total, there have been 9,418 reported cases of COVID-19 among people in Colorado’s state and federal prisons. As of this writing, there are 16,902 people held in state and federal prisons in Colorado. It’s difficult to say exactly how many people who are currently incarcerated have contracted COVID-19, since the prison population changes as people are admitted and released. But it’s safe to say that for every 1,000 prisoners in Colorado, 557 incarcerated people have been reported as COVID-positive.
Sterling Correctional Facility has experienced the largest outbreak of any prison in Colorado — as of January 20, 2021, 1,460 inmates had contracted COVID-19. The Arkansas Valley and Bent County Correctional Facilities are close behind, with 948 and 897 cases among inmates, respectively.
Photo by Jared Winkler - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=66346424
Many states have struggled with the spread of the COVID-19 in their prisons, but research from The Marshall Project places Colorado among the top 10 states where the problem is most profound.
ICE Detention Facility
The ICE detention facility in Aurora has reported an ongoing outbreak of COVID-19. The ICE facility, which is run by a private prison company, confirmed its first case on May 30, 2020, nearly eight months ago, and the outbreak has been considered active since then. To date, the ICE facility has reported 151 cases among detained people and 122 cases among staff. At the time of this writing, 228 people were detained at this facility.
In an interview with The Denver Post, a man detained at the ICE facility reported that detainees were not given adequate personal protective equipment or appropriately separated from people who had tested positive for the virus, allegations that a spokesperson from the facility rejects.
Jails
Nineteen Colorado jails have reported outbreaks since the pandemic began. The largest reported outbreaks are at El Paso County Criminal Justice Center and the Van Cise-Simonet Detention Center in Denver. Both outbreaks are ongoing. To date, over 1,100 cases have been reported at each location, over 1,000 of which are among people detained at those facilities.
In December, the American Civil Liberties Union of Colorado filed a suit against the El Paso County sheriff for “[failing] in multiple ways to protect people in his custody from the substantial risk of serious harm and even death posed by the highly contagious virus,” including failing to provide masks or separate COVID-positive people from those who had tested negative.
Some advocates have also expressed concern that testing across Colorado jails has been inconsistent and insufficient and that CDPHE’s data on jails may therefore not accurately capture the full extent of the problem.
Other Correctional Settings
Another 52 outbreaks have been reported at locations classified as “other” correctional settings, including community corrections centers and residential treatment centers for justice-involved people with substance use disorders. In total, 1,178 cases and four deaths have been reported at these locations.
Equity, Policy, and the Road Ahead
The prevalence of COVID-19 in Colorado’s detention and corrections system is not only a public health issue — it’s also an issue of equity.
Research has shown pronounced racial discrimination throughout the criminal justice system, from the likelihood of arrest to the length of sentence for the same crime.
As a result, people of color are overrepresented in Colorado’s incarcerated population. Black and African American people make up 5% of Colorado’s overall population but 18% of those incarcerated in state prisons. Hispanic/Latinx people make up 22% of the state population but 31% of the state prison population. And American Indian and Alaska Native people make up 2% of the overall population but 4% of the state prison population.
In other words, the rampant spread of COVID-19 in Colorado prisons and jails falls disproportionately on Black, Latinx, and Native people — communities that have borne the brunt of the pandemic both inside and outside of the carceral system.
Colorado is not the only state to omit justice-involved people among priority populations in its vaccine distribution plan, but it’s in the minority. According to recent analysis from the Prison Policy Initiative, all but 10 states — Colorado, Alaska, Arkansas, Florida, Michigan, Oregon, South Carolina, South Dakota, Texas, and Wisconsin — have addressed incarcerated people (either explicitly or implicitly as part of a broader group) in their vaccine distribution plans.
Designating incarcerated people as a priority population is consistent with advice from public health experts. It can also mitigate the spread of COVID-19 in the greater community.
In Massachusetts, prison inmates have been among the first to receive vaccines.
“We used equity as a core principle in our recommendations,” explained Dr. Simone Wildes, an infectious disease specialist and member of the Massachusetts’ vaccine advisory group, in an interview with The New York Times. “We have had a lot of cases of COVID in the prisons, and we wanted to make sure those at highest risk were getting the vaccine first.”
Polis, too, has emphasized fairness and equity as central tenets of Colorado’s vaccine distribution plan. But the omission of incarcerated people in the state’s vaccine distribution plan represents a departure from that stated goal.
Enormous harm has already fallen upon incarcerated and detained people in Colorado — harm that could have been prevented with better management of the pandemic, both in and outside of the detention and corrections system.
However, it is not too late to prioritize equity and data-informed public health responses as we forge our way to the other side of this pandemic. Centering equity and data in prevention, testing, vaccination, and long-term recovery efforts is not only a matter of principle — people’s lives depend on it.
Arkansas Valley Correctional Facility is one of six state prisons where the number of inmates infected with COVID-19 since the pandemic began exceeds more the 80% of the prison’s total inmate population. (The Four Mile, Arrowhead, Trinidad, Colorado Territorial, and Sterling Correctional Facilities also hold this distinction.) A total of 948 cases among inmates have been reported at Arkansas Valley, which, as of December 30, 2020, housed 990 inmates.
Photo by Jeffrey Beall - Own work, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=59712798
Sources
Unless otherwise noted, the figures cited in this report are based on publicly available data from the following sources and were up to date as of the dates noted below.
Data on COVID-19 cases and deaths in Colorado
Colorado Department of Public Health and Environment. COVID-19 Outbreak Data. Weekly report published January 20, 2021.
Data on COVID-19 cases and deaths in federal prisons
Federal Bureau of Prisons. COVID-19 Cases. Accessed January 22, 2021.
Data on state prison population
Colorado Department of Corrections. Monthly Population and Capacity Report. Last updated December 31, 2020.
Data on federal prison population
Federal Bureau of Prisons. Locations. Accessed January 22, 2021.
Data on Aurora Contract Detention Facility detainees
Office of Congressman Jason Crow. ICE Accountability Report. Electronic request completed January 13, 2021.
CHI staff contributing to this analysis
- Julia Char Gilbert (lead author)
- Kristi Arellano
- Joe Hanel
- Kimberly Phu
- Sara Schmitt
- Alec Williams