The Hospital Transformation Program
Key Takeaways
The Hospital Transformation Program (HTP), a new value-based care initiative in Colorado, will tie some Medicaid supplemental payments to hospitals’ ability to hit performance targets.
Over the five-year program, hospitals will earn that money by taking steps to improve the health of certain priority populations and to reduce costs.
It’s difficult to predict the HTP’s impact on hospitals and patients as many details about the program still need to be opened to public comment and approved by the federal government.
The Hospital Transformation Program (HTP) aims to improve outcomes and reduce costs by attaching quality and value metrics to the Hospital Provider Fee, a source of funding for most Colorado hospitals since 2009.
As of October 2, 2019, details of the HTP have not been finalized. CHI has drawn on publicly available materials and interviews with stakeholders to report on key points of the HTP as it is currently conceived, realizing provisions may change. CHI will continue to follow the HTP throughout its development and implementation.
Most public attention on health care costs this year focused on the legislature, which passed bills creating a reinsurance program and requiring the Department of Health Care Policy and Financing (HCPF) to produce annual reports on hospital finances and create a public option for health coverage, in cooperation with the Division of Insurance. The HTP, also a HCPF initiative, has attracted far less attention, even though the impact on hospitals could be as great as anything passed by lawmakers in the most recent session.
The HTP, which is tentatively scheduled to be implemented in April 2020, is a five-year care delivery and payment reform effort involving general acute care hospitals participating in Health First Colorado (Colorado’s Medicaid program). It’s a critical piece of a broader push for reduced health care costs by HCPF, which runs Medicaid. Over the course of the program, 76 hospitals will be eligible to earn back at-risk dollars for meeting patient care performance targets and for drawing on community insight to design and implement initiatives addressing the unique health needs of their patient population.
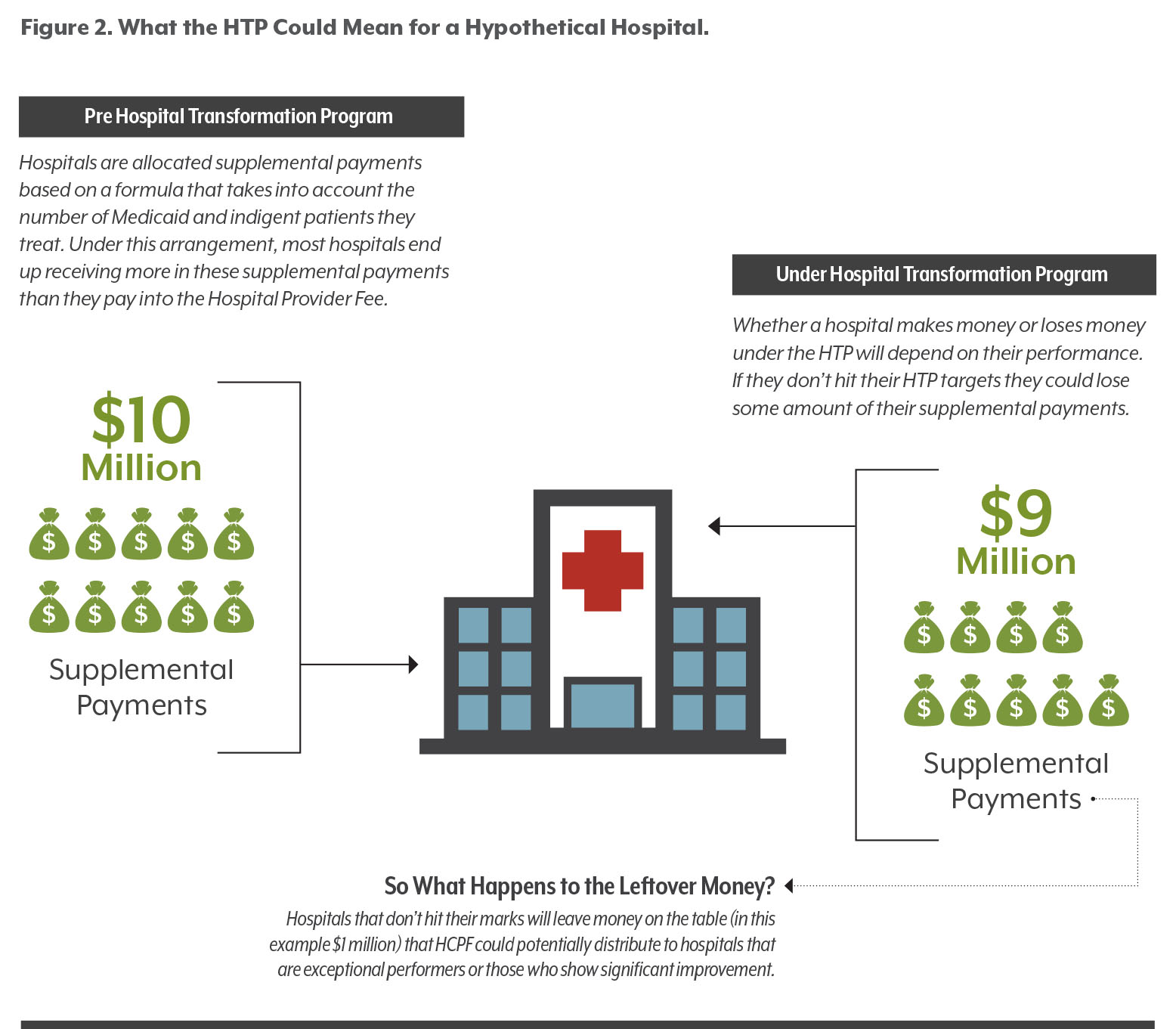
This means hospitals are in for a change. The Hospital Provider Fee program pays hospitals based on a formula that considers the number of Medicaid and indigent patients they treat. But under the HTP, hospitals could be penalized or rewarded based on whether they hit performance targets or create savings.
The details of those targets matter greatly to hospitals and to the success of the HTP. The final targets are still being discussed. The draft scoring framework proposed by HCPF will measure hospitals’ performance in the following focus areas:
- Avoidable inpatient and outpatient hospitalizations;
- Vulnerable populations (including pregnant women and people whose health is worsened by their environment);
- Behavioral health and substance use disorder;
- Clinical and operational efficiencies; and
- Population health and total cost of care.
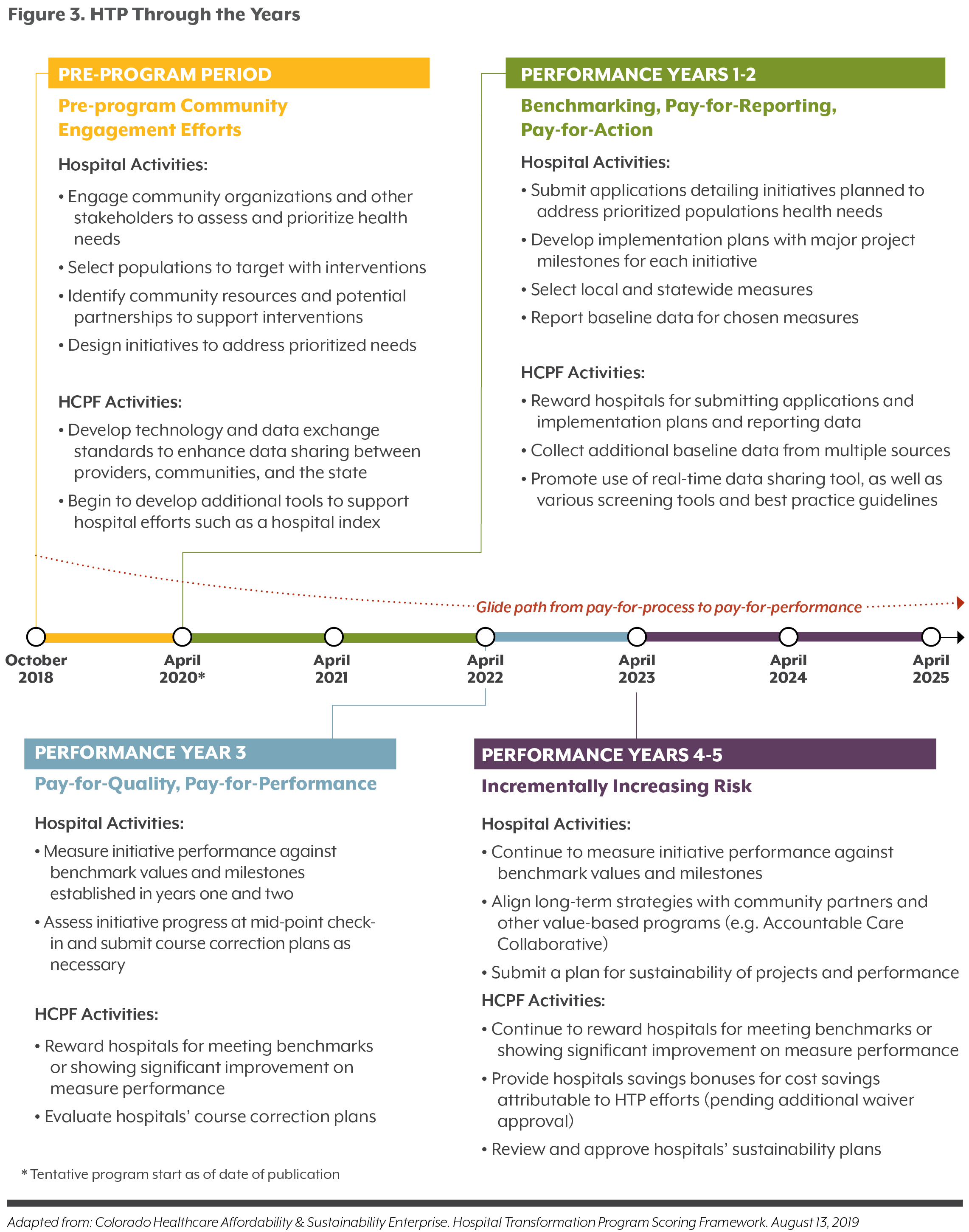
In early years, hospitals will earn HTP payments by laying the groundwork for reform. Hospitals will identify target patient populations and opportunities for intervention, design and implement initiatives to improve the health of those patients, and report on their progress. In later years, payments increasingly will be tied to demonstrating success in transforming care, improving population health, and reducing costs.
In addition to improving patient outcomes, the HTP is intended to reduce Medicaid costs by incentivizing hospitals to operate more efficiently and effectively. This could mean, for example, better managing care for patients with chronic or complex needs and expansion of telemedicine, in addition to other approaches identified by hospitals and their community stakeholders.
How Did We Get Here?
In 2009, the legislature passed a bill creating the Hospital Provider Fee, an assessment on hospitals that is matched dollar for dollar with federal money. Legislation passed in 2017 moved administration of the provider fee to the Colorado Healthcare Affordability and Sustainability Enterprise (CHASE), a government-owned business within HCPF. It also instructed CHASE to work with hospitals to create a payment reform initiative, laying the groundwork for what would become the Hospital Transformation Program.
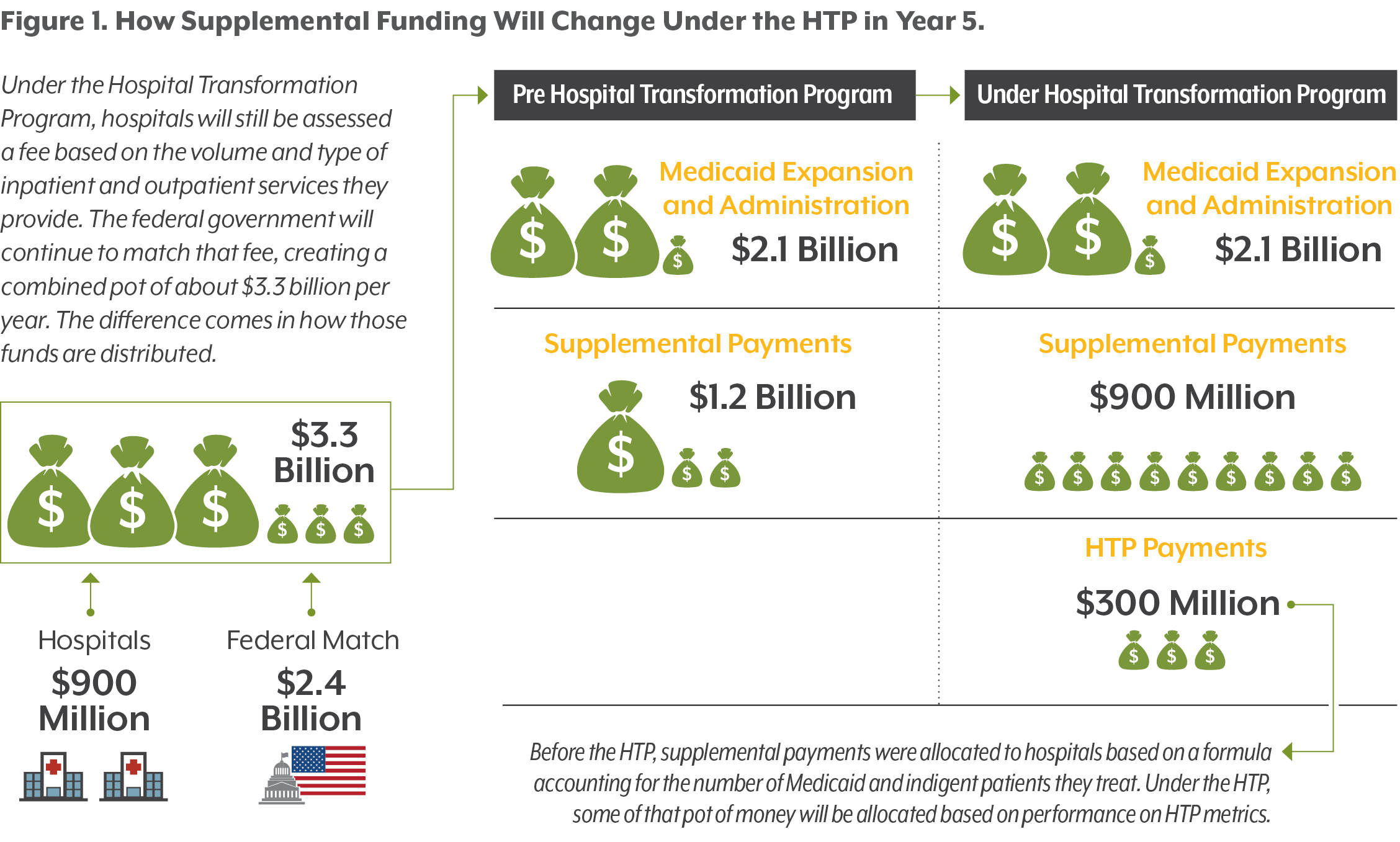
Some hospital provider fee dollars cover the costs of insuring Colorado’s Medicaid expansion population; some are returned to hospitals in the form of supplemental payments based on the type of hospital, how much care it provides to Medicaid patients and the uninsured, and how sick its patients are. Under this arrangement, most hospitals end up receiving more in supplemental payments than they pay into the Hospital Provider Fee.
In Fiscal Year 2017-18, Colorado hospitals paid about $900 million to the Hospital Provider Fee, which was matched with federal funds to create a combined pot of about $3.3 billion. Of that pot, hospitals received about $1.2 billion in supplemental payments. The remainder, about $2.1 billion, finances Colorado’s expansion in Medicaid eligibility and pays for administrative costs. Of the $1.2 billion in supplemental payments, about $1 billion could be tied to hospital participation in the HTP. Until the program is finalized, particulars are subject to change. But, most of that $1 billion will not actually be at risk for hospitals, especially in early years of the program.
A proposal from HCPF says participating hospitals could lose 5 percent of their supplemental payment in year one of the program, rising incrementally each year and topping out at 30 percent in year five. This would mean the risk for hospitals in dollars would ultimately be $300 million of the total $1 billion distributed in supplemental payments. And not all of those at-risk dollars will be tied directly to improvements in care quality or reductions in cost — hospitals will be able to earn some of their at-risk dollars by meeting process measures like reporting data to HCPF on time, creating a sustainability plan outlining how HTP-related activities will continue past the end of the program, and meeting other major HTP milestones. Hospitals that don’t hit their marks will leave money on the table that HCPF intends to distribute to those that do. Every year the HTP progresses, the amount of money hospitals stand to lose for missing their goals increases.
The HTP joins other Colorado efforts to tackle Medicaid payment and delivery reform, such as the Accountable Care Collaborative (ACC). But the HTP could be the most significant effort so far to shift the way care is paid for and delivered and is the first mandatory state-driven program of its kind for hospitals.
This particular setting is vital: Hospital costs account for 34 percent of health care spending in Colorado, and 30 percent ($2.7 billion) of Medicaid spending. Every year, hospitals deliver inpatient care to half a million Coloradans and provide 9 million outpatient visits, according to the Colorado Hospital Association.
Keeping Track of the Terms
Hospital Provider Fee: An assessment on hospitals, started in 2009, based on the volume and type of inpatient and outpatient services they provide. A hospital’s assessment is capped at six percent of net patient revenues. The fee is matched with federal funds from the Centers for Medicare and Medicaid Services. Some of the fee money is used to finance Medicaid expansion and to pay the costs of administering the fee. The majority, plus the federal match dollars, is distributed to hospitals. It is still referred to as the “Hospital Provider Fee” but officially known as the Healthcare Affordability and Sustainability Fee.
Colorado Healthcare Affordability and Sustainability Enterprise (CHASE): An entity within HCPF charged with collecting and distributing the Hospital Provider Fee. CHASE is governed by a 13-member board that includes state, hospital, and other community and industry representatives appointed by the governor.
Colorado Department of Health Care Policy and Financing (HCPF): The state agency that oversees Colorado’s Medicaid program (Health First Colorado) and administers the Accountable Care Collaborative, CHASE, and the HTP.
Accountable Care Collaborative (ACC): A Medicaid program, launched in 2014, designed to improve coordination of primary and behavioral health care for almost 1.2 million Medicaid beneficiaries in Colorado.
Regional Accountable Entities (RAEs): Seven organizations charged with carrying out ACC activities for the participating Medicaid beneficiaries in their region. They are required to assist hospitals with some HTP activities.
Where Are We Now?
In preparation for the start of the HTP, HCPF required hospitals to ask a wide variety of community stakeholders — including their Regional Accountable Entity (RAE), local public health agencies, community health centers, providers, and community organizations — about health-related needs in the area. The environmental scan required hospitals to assemble focus groups, conduct interviews, and gather quantitative data about demographics of their patients and their health needs. (Several Denver-area hospitals contracted with the Colorado Health Institute to do this work.)
The community engagement process and environmental scan (called the “Community and Health Neighborhood Engagement” process) was meant to give hospitals a better understanding of their patients, their community, their area’s health problems, and the types of organizations and services available to help them. The scan was intended to focus on HTP priority populations, as well as Medicaid enrollees and uninsured people. Information gathered during this process is meant to help hospitals pick the problems they want to solve and the initiatives they design to solve them during the HTP.
The initial environmental scan process was completed at the end of September, when hospitals submitted final reports on their findings to HCPF. But the engagement is not supposed to stop there. HCPF plans to use the HTP to get hospitals to increase their outreach beyond their walls by continuing to participate in discussions around health needs in the community and helping to coordinate care transitions and data sharing as patients are discharged.
Where Are We Headed?
HCPF is targeting April 1, 2020, as the start date for the HTP. This fall, HCPF plans to submit details of the program for public comment, then submit them by the end of the year to the Centers for Medicare & Medicaid Services (CMS) for approval. HCPF intends to implement the program once CMS approves. That approval could happen as early as March, but a delay in receiving approval from CMS could push the implementation to a later date.
In the first two years of the program, hospitals will earn payments for reporting patient care data and submitting their application materials and implementation plans to HCPF. Hospitals are asked to identify milestones for activities they plan to perform in the first two years. They also must continue and report on community engagement activities. The focus will be on establishing groundwork and gathering baseline data for benchmarking against performance in future years. Starting in the third year of the program, hospitals may have to meet performance benchmarks in addition to hitting milestones and satisfying reporting requirements in order to earn their full payments. Hospitals that fall short of their benchmarks may be able to reduce their penalty by showing improvement.
Each of the five areas of focus for the HTP has an associated set of metrics. For each focus area there will be at least one metric required of most hospitals by the state, as well as a list of additional metrics (called local measures) for hospitals to choose from. HCPF intends for hospitals to choose local measures that reflect community needs uncovered during their public engagement process. The number of metrics required may depend on hospital size and specialty type. Larger hospitals will be accountable for more metrics than smaller hospitals, while specialty hospitals (such as pediatric hospitals) may have their requirements tailored to their patient populations.
For example, for the focus area of behavioral health and substance use disorder, many hospitals may be tracked on their use of alternatives to opioids in the emergency department through a statewide measure. Hospitals that identified substance use disorder as a priority for their community in the public engagement process may also choose to be graded on a local measure, such as increasing initiation of Medication-Assisted Treatment in the emergency department.
Federal Approval
Part of the authority for the HTP comes from a Medicaid State Plan Amendment (SPA), which states submit to CMS for approval of certain limited changes to their Medicaid programs. The SPA process is typically shorter and less resource intensive than other routes states can take. But states are limited in the changes they can make through the SPA process, meaning HCPF can accomplish some but not all its goals for the HTP under SPA authority alone.
To fully implement certain components of the program, HCPF will need waiver approval from CMS. Those components include providing bonus payments to hospitals that generate savings by reducing unnecessary care and making certain investments in rural infrastructure. Those components of the program do not phase in until year 3 of the program, meaning HCPF could start the HTP before the additional federal approval comes through. At this time however, HCPF intends to submit for approval via both routes simultaneously and begin the program once both approvals are received.
How Does HTP Fit in With Other State Programs?
The HTP is one of a number of ongoing statewide efforts with similar overarching goals, and it must interact with several of those programs.
In 2018, HCPF created seven Regional Accountable Entities (RAEs) responsible for coordinating primary and behavioral health care for almost 1.3 million Medicaid beneficiaries. The RAEs are part of the Accountable Care Collaborative (ACC), an ongoing effort to reduce costs and improve quality in Medicaid that has shown modest cost savings for the state so far.
The RAEs’ focus is on the care patients receive in settings outside hospitals, but they are also required to partner with hospitals in their region as part of the HTP. RAEs are responsible for defining the “Community and Health Neighborhood” that hospitals may consult during the public engagement process. This means helping to identify and organize community stakeholders who will share information with hospitals about community needs and resources. RAEs also perform a variety of functions that overlap with the HTP, such as helping hospitals improve care transitions, address complex health needs, and maintain and share data sets on patients, local provider networks, community resources, and more.
As hospitals design and implement initiatives that reach beyond their walls, the RAEs will be a key resource for connecting them with their communities.
Other value-based programs already at play in the state include the Medicaid Primary Care Alternative Payment Model, Comprehensive Primary Care Plus, and the Hospital Quality Incentive Payment (HQIP) Program. These efforts, with the exception of HQIP, focus on care delivered outside of hospitals. HCPF intends to use the HTP as an incentive for hospitals to align their operations, partnerships, data sharing and infrastructure with the work going on in these programs (or their successors) and with the efforts of the community partners.
As part of that alignment, HCPF intends to use the HTP as a vehicle for incentivizing the adoption of various technology, processes, and protocols. These are intended to further the HTP’s overarching goal of transforming care through improved care integration, coordination, efficiency, quality and value.
Certain efforts, such as an advanced care plan repository, are required by existing legislation, but could also be a requirement for earning HTP payments. Other efforts, like a planned data sharing tool, could be developed and tied to the HTP. If it works, this tool would allow hospitals, other providers, community organizations, and the state to share data in real-time. However, technical challenges and a lack of incentives for hospitals have thus far prevented the development of a system that allows data to be easily shared. It’s not clear whether the HTP will enable HCPF to achieve this ambitious goal.
Will the HTP Transform Hospital Care in Colorado?
Success for the HTP, according to the vision laid out in a concept paper published by HCPF in January, means improved patient outcomes, lower Medicaid costs, and increased readiness for a future where value-based care is the standard.
Achieving those goals may require hospitals to invest significant time and resources in interacting with their community, then designing and executing meaningful projects. It may also require them to take a more active role in coordinating patient care outside of the hospital by working with primary care providers, RAEs, and other community organizations. The public engagement process was designed to bring together these stakeholders to form working relationships. How those working relationships evolve will be crucial to the success of the program.
Will the HTP transform hospital care in Colorado? Maybe — but it’s too early to tell. What will the program look like after going through the public comment and CMS approval processes? Which metrics will hospitals choose? When will the bonus savings kick in? Will the partnership between HCPF and hospitals lay the groundwork for more ambitious collaborative efforts to tackle population health and reduce total cost of care, as HCPF intends? The answers to these questions could have a major effect on the cost and quality of health care in Colorado.
For the latest updates on the Hospital Transformation Program visit:
colorado.gov/pacific/hcpf/colorado-hospital-transformation-program
CHI Staffers Contributing to This Report:
• Spencer Budd, Lead Author
• Jeff Bontrager
• Ashlie Brown
• Brian Clark
• Joe Hanel
• Cliff Foster
• Emily Johnson
• Michele Lueck
• Sara Schmitt
• Jackie Zubrzycki