Endnotes
1 Taylor LA, Coyle CE, Ndumele C, Rogan E, Canavan M, Curry L, et al. “Leveraging the Social Determinants of Health: What works?” Blue Cross Blue Shield of Massachusetts Foundation; (June 2015). http://bluecrossfoundation.org/sites/default/files/download/publication/Social_Equity_Report_Final.pdf
2 Agency for Healthcare Research and Quality. (December 2016). “Clinical-Community Linkages.” https://www.ahrq.gov/professionals/prevention-chronic-care/improve/community/index.html.
3 Agency for Healthcare Research and Quality. (December 2016). “Clinical-Community Linkages.” https://www.ahrq.gov/professionals/prevention-chronic-care/improve/community/index.html.
4 Centers for Disease Control and Prevention. “What Is the National DPP?” January 14, 2016. https://www.cdc.gov/diabetes/prevention/about/index.html.
5 National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, U.S. Department of Health and Human Services. “Diabetes Prevention Program (DPP).” (October 2008). https://www.niddk.nih.gov/about-niddk/research-areas/diabetes/diabetes-prevention-program-dpp/Documents/DPP_508.pdf.
6 Colorado Department of Public Health & Environment. “Diabetes Prevention Program.” https://www.colorado.gov/pacific/cdphe/diabetes-prevention-program. Accessed July 18, 2017.
7 Health & Human Services Press Office. “Independent experts confirm that diabetes prevention model supported by the Affordable Care Act saves money and improves health.” March 23, 2016. https://wayback.archive-it.org/3926/20170127185647/https://www.hhs.gov/about/news/2016/03/23/independent-experts-confirm-diabetes-prevention-model-supported-affordable-care-act-saves-money.html
8 Centers for Medicare & Medicaid Services. “Medicare Diabetes Prevention Program (MDPP) Expanded Model.” November 2, 2016. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-11-02-2.html.
9 Nurse Family Partnership. “Nurse Family Partnership of Colorado.” http://www.nursefamilypartnership.org/locations/Colorado. Accessed July 13, 2017.
10 Tri-County Health Department. “Nurse Family Partnership.” http://www.tchd.org/352/Nurse-Family-Partnership. Accessed July 13, 2017.
11 Nurse Family Partnership. “State Profile: Nurse Family Partnership in Colorado.” http://www.nursefamilypartnership.org/assets/PDF/Communities/State-Profiles/CO_State_Profile.aspx. Accessed July 13, 2017.
12 Colorado Department of Public Health & Environment. “Community-clinical Linkages.” https://www.colorado.gov/cdphe/domain-4-community-clinical-linkages. Accessed July 18, 2017.
13 Barbare, S. “Colorado works to establish registry for patient navigators.” Colorado Department of Public Health and Environment. https://www.colorado.gov/pacific/cdphe/news/patient-navigator-registry. Accessed July 18, 2017.
14 Colorado Patient Navigator / Community Health Collaborative. “Welcome to the Colorado Community Health Worker and Patient Navigator Work Group.” https://sites.google.com/site/copnchwcollaborative/home. Accessed July 18, 2017.
15 No Kid Hungry, Center for Best Practices. “Fighting Hunger Through Health Care: A Seamless Solution.” (September 1, 2012).
https://bestpractices.nokidhungry.org/sites/default/files/resources/Health%20Care%20Issue%20Brief.pdf.
16 The Healthy Start Study. https://healthystartstudy.org/healthy-start-i/. Accessed July 18, 2017.
17 CC Relationships Evaluation Roadmap AHRQ July 2013
18 Shelley, D, Cantrell J. “The effect of linking community health centers to a state-level smoker’s quitline on rates of cessation assistance.” BMC Health Services Research 10 (2010): 25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2823740/. Accessed April 18, 2018.
19 Porterfield, D et al. “Linkages Between Clinical Practices and Community Organizations for Prevention: A Literature Review and Environmental Scan.” American Journal of Public Health 102 (June 1, 2012): S375-S382. https://ajph.aphapublications.org/doi/abs/10.2105/AJPH.2012.300692?url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org&rfr_dat=cr_pub%3Dpubmed. Accessed April 18, 2018.




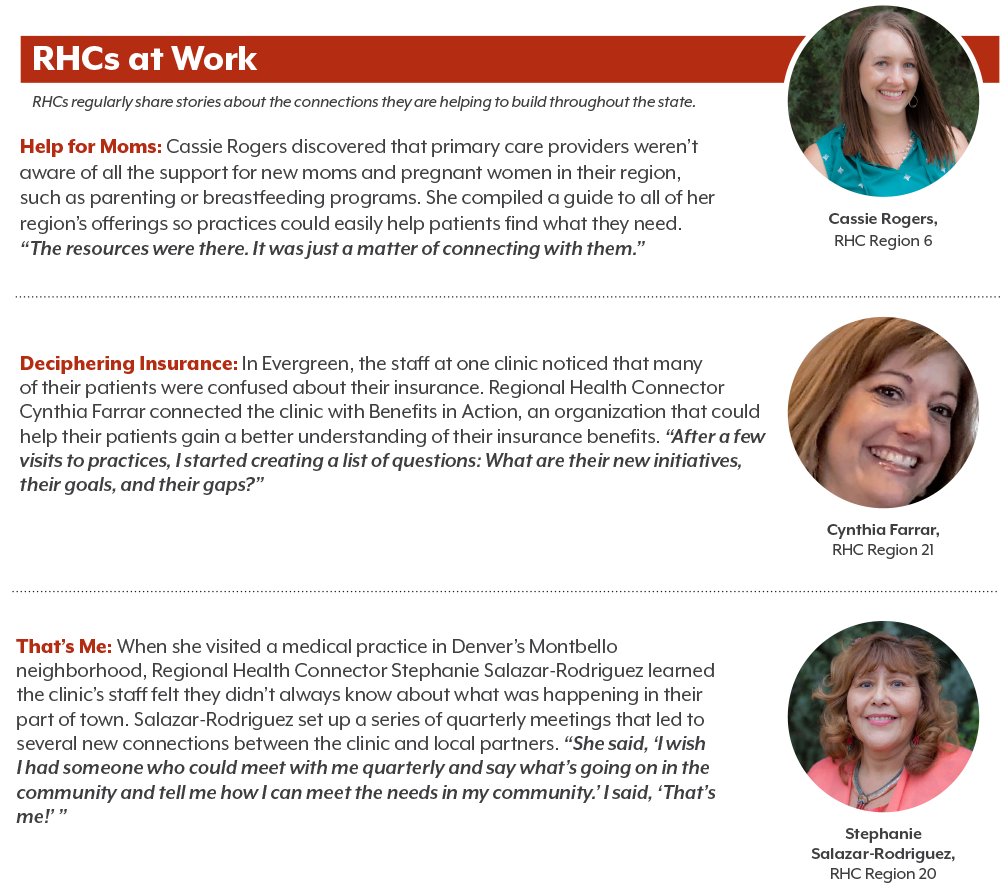
 RHCs connect clinics and community groups to advance health and address the social determinants of health. They do this by improving the coordination of services and strengthening ties among health care providers and others outside their offices, whether by forging a relationship between a clinic and the local food bank or connecting a hospital system with community-based chronic disease management programs.
RHCs connect clinics and community groups to advance health and address the social determinants of health. They do this by improving the coordination of services and strengthening ties among health care providers and others outside their offices, whether by forging a relationship between a clinic and the local food bank or connecting a hospital system with community-based chronic disease management programs.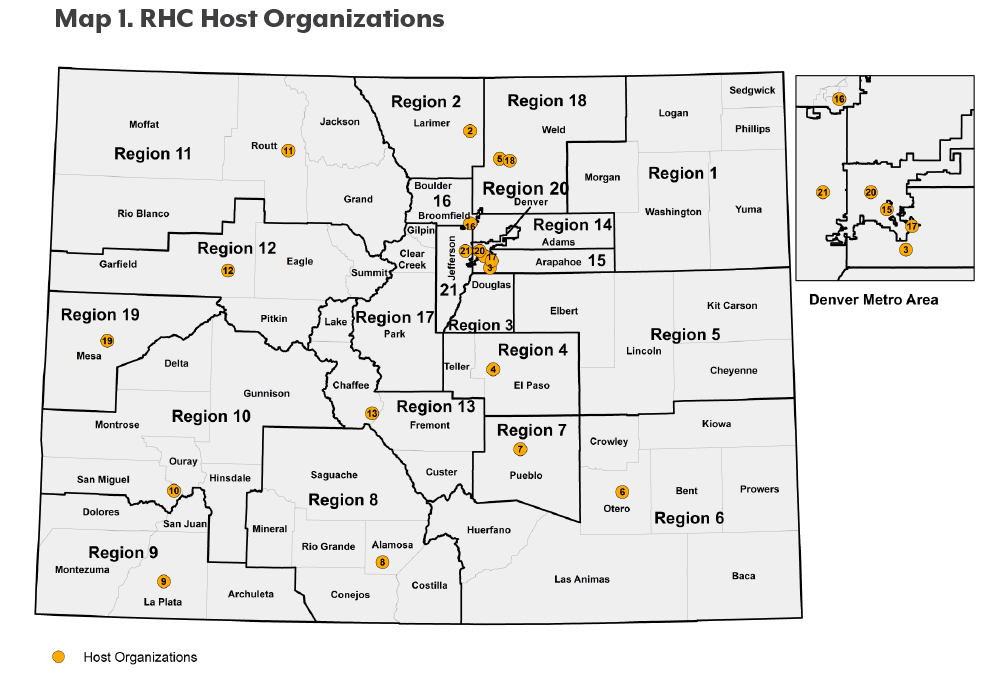
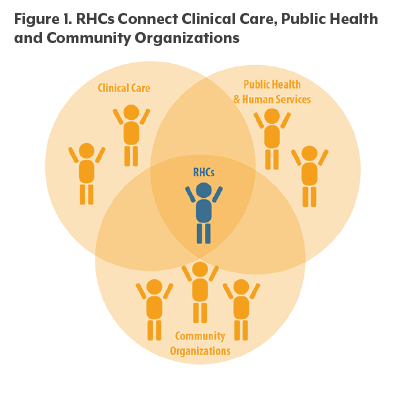 RHCs are a unique new workforce that builds upon this work in a systematic way throughout Colorado. RHCs are dedicated to improving the coordination of services to address the social determinants of health. Supporting and strengthening clinical-community linkages across the state is a major part of their jobs.
RHCs are a unique new workforce that builds upon this work in a systematic way throughout Colorado. RHCs are dedicated to improving the coordination of services to address the social determinants of health. Supporting and strengthening clinical-community linkages across the state is a major part of their jobs.