Colorado’s Opportunity
Six of the eight hottest years on record in Colorado have happened in the past decade.4 Colorado’s average temperature has increased by about 2 degrees Fahrenheit in just the past 30 years.5 Projections suggest it could increase by an additional 2.5 to 5 degrees Fahrenheit by 2050.5 Residents of Colorado’s urban and suburban areas — where a majority of the state’s population resides — see and feel days of poor air quality each year. Denver-Aurora, Fort Collins, and Colorado Springs rank among the worst metropolitan areas in the United States for air pollution, particularly for ozone, which can irritate the lungs and exacerbate chronic health conditions. In fact, in 2021, the Denver metro area recorded a record 65 ozone alert days from May through August — the four months of the ozone season.6
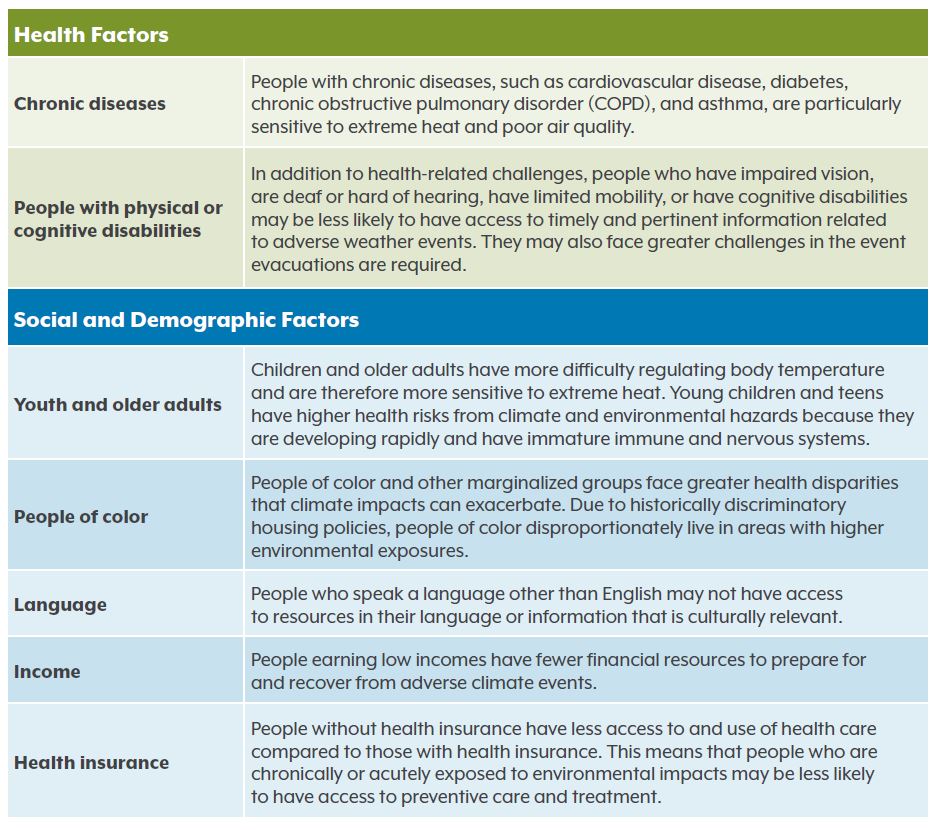
Southern and southeastern Colorado continue to face extreme drought conditions, affecting local food and economic security and the mental health of local communities.7 These areas are home to some of the more sensitive populations such as adults over 65 years old, people with chronic diseases, people who are housing insecure, and households earning a low income.
Climate change is a health equity issue. Health systems — including their health care delivery, workforce, research, and philanthropic divisions — have an opportunity to take a lead role in tackling the climate crisis. Addressing climate change is similarly aligned with philanthropic organizations’ and health foundations’ commitment to advancing racial equity, environmental justice, and health. Coloradans are already feeling the health impacts of climate change and need leaders from the health care and philanthropic sectors to help address them.
Building community resilience to climate change is essential for preserving the physical and mental health of Coloradans, especially for people of color, immigrant groups, households earning low-incomes, children, and older adults who are particularly sensitive to climate change impacts due to chronic conditions and physical vulnerabilities.
Many agencies and organizations across Colorado are working to address climate change, and many more are interested in and positioned to join and advance these efforts. Health systems and philanthropic organizations are recognizing their role as environmental stewards with a responsibility to protect the natural environment and human health, which are interconnected and interdependent. Health care and philanthropic groups have an opportunity to leverage their resources, infrastructure, workforce, and community connections to foster healthy, thriving, and resilient communities.
This report presents a call to action to health systems and philanthropic organizations to learn about and pursue opportunities to protect and advance the health and well-being of communities from the impacts of climate change in Colorado.
Background and Methods
Kaiser Permanente Colorado commissioned the Colorado Health Institute (CHI) to identify recommendations for health systems and philanthropic organizations to support, lead, and advance climate change mitigation and adaptation efforts in Colorado.
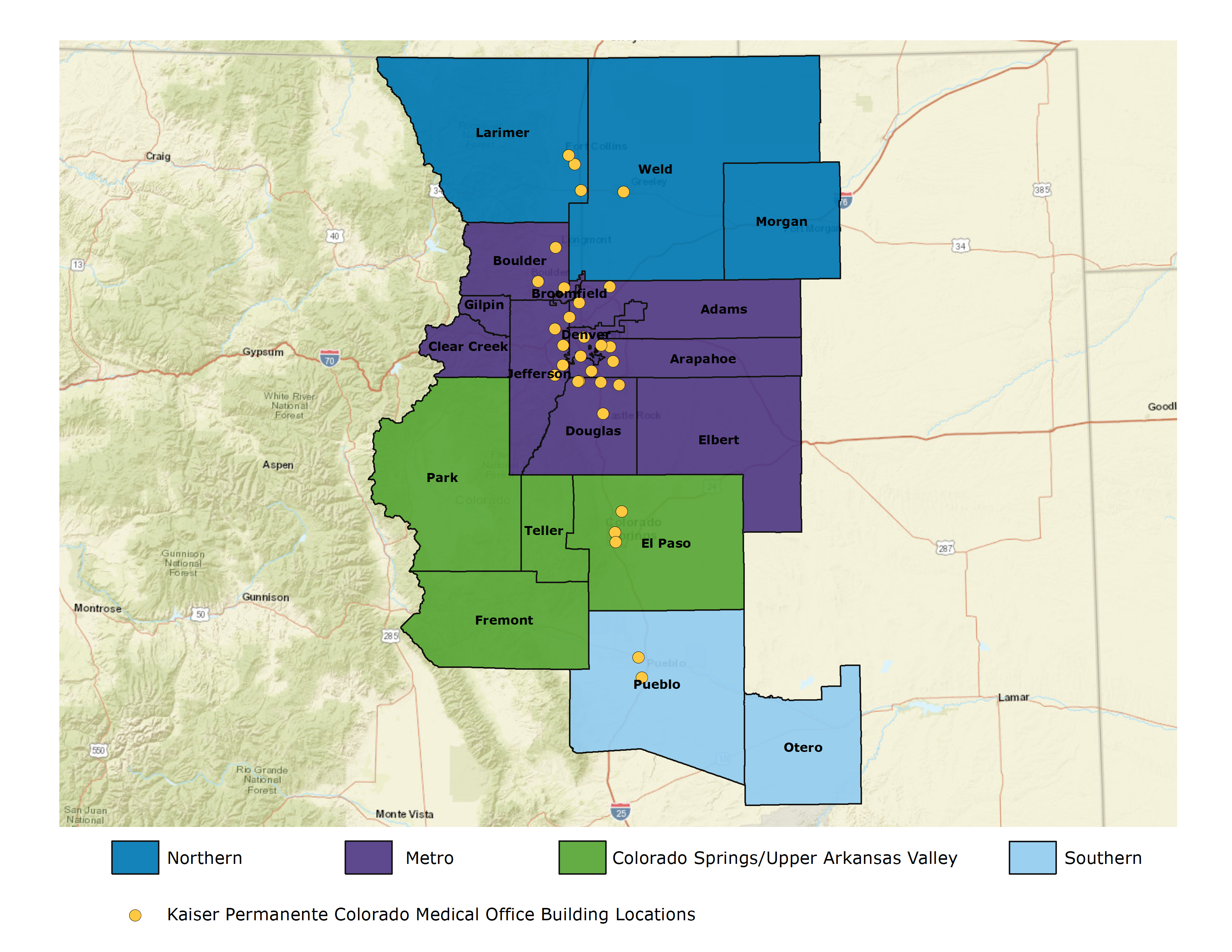
For its assessment, CHI collected and analyzed data to identify and map needs within each of Kaiser Permanente Colorado’s service areas, then conducted a landscape scan of existing programs, needs, and opportunities across those areas (Map 1) to inform the recommendations included in this report.
While not inclusive of the state’s entire geography, Kaiser Permanente Colorado’s service area encompasses a majority of Colorado’s population at nearly 5 million people (or 86% of Colorado residents).