
2019 Medicaid and Commercial Access to Care Index
How Payer Type Influences Coloradans’ Access to Needed Health Care
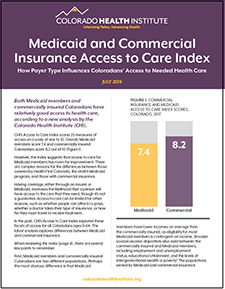
Both Medicaid members and commercially insured Coloradans have relatively good access to health care, according to a new analysis by the Colorado Health Institute (CHI).
CHI’s Access to Care Index scores 25 measures of access on a scale of one to 10. Overall, Medicaid members score 7.4 and commercially insured Coloradans score 8.2 out of 10.
However, the index suggests that access to care for Medicaid members has room for improvement. There are complex reasons for the differences between those covered by Health First Colorado, the state’s Medicaid program, and those with commercial insurance.
Having coverage, either through an insurer or Medicaid, increases the likelihood that a person will have access to the care that they need, though it’s not a guarantee. Access to care can be limited for other reasons, such as whether people can afford co-pays, whether a doctor takes their type of insurance, or how far they must travel to receive treatment.
In the past, CHI’s Access to Care Index explored these facets of access for all Coloradans ages 0-64. The latest analysis explores differences between Medicaid and commercial insurance.
When reviewing the index, there are several key points to remember.
First, Medicaid members and commercially insured Coloradans are two different populations. Perhaps the most obvious difference is that Medicaid members have lower incomes on average than the commercially insured, as eligibility for most Medicaid members is contingent on income. Broader socioeconomic disparities also exist between the commercially insured and Medicaid members, including employment and unemployment status, educational attainment, and the levels of intergenerational wealth or poverty.(1) The populations served by Medicaid and commercial insurance also differ demographically. Medicaid serves a disproportionate number of pregnant women, older adults, and people with complex medical conditions and disabilities when compared with the state’s population.(2)
Second, the health care services covered vary between the two types of coverage. For example, Health First Colorado’s dental benefit varies by age of the member. Benefits covered by commercial plans tend to vary by how much customers are willing to pay for insurance, or if they are covered by employer-sponsored or individual plans.
In addition, access to specific services may differ across payers as well. CHI’s recent analysis of access to specialty care services estimated that 486,000 specialty care visits go unmet among Medicaid members when compared to Coloradans with commercial insurance.(3)
Third, context is important. A national study comparing Medicaid members and commercially insured people found access among both groups is relatively high across the country, particularly in comparison to those who are uninsured.(4) In Colorado, access continues to be a challenge for the approximately 6.5 percent of people without insurance.(5) Moreover, access to care may not directly correlate to satisfaction with coverage. Colorado Medicaid members report high levels of satisfaction with their health services, scoring some components even higher than ratings reported by people with private insurance.(6)
Given these considerations, the index can be used to discuss and act on broader inequities in society that discourage people from obtaining the care they need, such as time-off policies that disproportionately impact low-wage workers or how people are treated when they step into a doctor’s office. It is intended to be a conversation starter for health policy changes that improve access to care.
Want to learn more about the Access to Care Index?
Text Continues Below
var divElement = document.getElementById('viz1562701737845'); var vizElement = divElement.getElementsByTagName('object')[0]; vizElement.style.width='1100px';vizElement.style.height='1127px'; var scriptElement = document.createElement('script'); scriptElement.src = 'https://public.tableau.com/javascripts/api/viz_v1.js'; vizElement.parentNode.insertBefore(scriptElement, vizElement);
Measuring Access to Health Care: Observations from the Index
The Access to Care Index aims to synthesize — at the state and county level — the many factors that contribute to access to care. It features three domains of access — potential access, perceptions/experiences, and realized access — with a total of 25 metrics. (See Methods and Metrics on Page 3). CHI calculated an overall access score for each county as well as a score for each of the domains.
The Access to Care Index is available as an interactive dashboard on CHI’s website. Several types of comparisons are possible: comparisons by payer, by geography, and by domain. Dashboard users can examine access at the local level, comparing one county to another, and use the index at a state level to consider policy changes that address specific barriers to health care.
Potential Access: Coloradans with commercial insurance have a better chance of finding a provider
Obtaining health care is difficult if there isn’t a sufficient network of providers. Availability varies by geography and by payer. Coloradans with commercial insurance tend to have more choices about where they can obtain care.
In particular, the number of commercially insured Coloradans for every primary care doctor is lower than the number of Medicaid members for every primary care physician who accepts Medicaid (Figure 3).
There is even less availability of dentists for Medicaid members than for people with commercial insurance, despite an expansion of Medicaid dental benefits to adults in 2014.
Last year, one in five (21.5 percent) Medicaid members reported being turned away from care due to their insurance. Among the commercially insured, just 6.7 percent of people reported this happening.(7) Why?
One reason is that providers do not have to accept Medicaid. At the national level, physicians often cite lower reimbursement rates compared with Medicare and commercial insurance. Other factors cited by providers nationally include delays getting paid and the administrative burden of working with Medicaid.(8,9)
In Colorado, the evidence is limited on providers’ attitudes toward Medicaid reimbursement. However, reviews of reimbursement rates by the Colorado Department of Health Care Policy and Financing (HCPF) in 2018 and 2019 found that Medicaid’s reimbursement rates for primary care, on average, were 85.09 percent of a benchmark derived from Medicare and similar states; and fee-for-service behavioral health rates were 94.67 percent compared to the benchmark states. Colorado’s Medicaid reimbursement for dental services was generally at or above the reimbursement levels of a selected group of similar states.(10)
Even providers who accept Medicaid might take only a small number of patients covered by the program. According to the Colorado Health Access Survey, Medicaid members were more than twice as likely as people with commercial insurance to report that their provider of choice was not accepting new patients.
However, not all people with commercial insurance enjoy high levels of access to providers. For example, after major provisions of the Affordable Care Act (ACA) went into effect in 2014, many insurance companies narrowed their networks of providers in an effort to control costs. This represented less choice of providers for consumers, particularly those who purchase plans directly from a carrier through the health exchanges.(11) Colorado’s Division of Insurance adopted network adequacy criteria in 2016 that include maximum travel distance standards, appointment wait times, and provider-to-enrollee ratios.(12)
Perceptions and Experiences: Regardless of payer, most people have a usual source of care. But the logistics of getting to the doctor are harder for Medicaid members.
Most Coloradans — about 84 percent across all age groups — report having a usual source of care, such as a primary care office, that is not an emergency room.(13) Having a primary care doctor is particularly important for managing chronic or complex health conditions. Of the one in five Coloradans who say they don’t have a usual source of care, the most common reason they give is not having health issues that require professional treatment.
Despite this good news, many people still have a hard time getting in to see a doctor, especially Medicaid members, who often face income-related constraints.
For instance, Medicaid members are more likely than those with commercial insurance to report not getting care because of the difficulty of finding child care (Figure 4). They’re also twice as likely to say they skipped medical care because they couldn’t take time off work.
These barriers to health care are not directly related to enrollees’ Medicaid coverage. Rather, systemic factors make it harder for people with lower incomes to access the care they need.
For example, just two in five Coloradans have access to paid sick leave through their jobs, and low-wage earners and people of color, particularly Latinx Coloradans, are most likely to lack this benefit.(14,15) Without paid sick leave, a person may have to forgo a day’s worth of wages just to see a doctor.
Medicaid members also are more likely than people with commercial insurance to report that transportation limits their access to needed care (13.8% versus 1.5%). Getting from home to the doctor’s office can be difficult due to the costs of travel and the time it takes. Coloradans with lower incomes, rural residents, and Latinx and African Americans are disproportionately impacted.(16) However, transportation challenges are faced by urban Medicaid members, too. Denver County had the largest percentage of enrollees reporting transportation was a barrier to getting needed care. One reason may be that public transit isn’t easily available to everyone and costs more than other cities.(17) And although Medicaid — unlike commercial insurance — provides a non-emergency transportation benefit to members who are unable to secure a ride to a medical appointment, some member advocates have cited missed appointments or long wait times for a ride with the state’s transportation contractors.(18)
Cost is another barrier worthy of attention. The Colorado Health Access Survey suggests that the cost of care, even for Medicaid members, prevents some people from keeping medical appointments (Figure 5). This is especially true for dental care.
Medicaid members reported greater cost concerns than commercially insured people despite not paying health insurance premiums and having limited co-pays. This is an area ripe for future research. One reason may be that Medicaid doesn’t cover all health services, such as eye exams and glasses. Another reason may be the comprehensive costs of seeking care as a low-wage earner.(19) Seeing a doctor sometimes means a day without pay, plus other costs such as gas or bus tickets and co-pays. Moreover, Medicaid members in Colorado report lower levels of being treated respectfully by providers than those with commercial insurance. That total experience can be costly both financially and in terms of time and stress.(20)
Health First Colorado enrollees are not the only Coloradans expressing cost concerns. People who buy their own insurance are more likely than all other types of insurance — including Medicaid — to skip medical care due to cost concerns.(21)
Realized Access: Regardless of payer, actually obtaining preventive care remains hardest.
Obtaining care, such as getting a mammogram or dental cleaning, is not a given. Even if people are insured, have providers available, and can get past challenges, such as the cost of care, they still may not get the treatment they need. This is true of both commercially insured people and Medicaid members.
People may not seek preventive care and instead wait until a minor problem gets worse. Rates of realized access also may be low due to the accumulation of barriers cited in the previous two domains.
There is room for improvement in realized access for commercially insured people and Medicaid members. However, for those enrolled in Medicaid, better access is particularly needed because use of preventive services is even lower than for the commercially insured. For example, nearly two-thirds of commercially insured women get the recommended breast cancer screening but just 42 percent of women enrolled in Medicaid are screened (Figure 6). As discussed elsewhere, Medicaid members may face additional economic and logistical challenges that make it difficult for them to follow through on a referral for a needed screening.
The Colorado Department of Health Care Policy and Financing has strategies to boost the use of preventive services and screenings among Health First Colorado members. For example, the Regional Accountable Entities (RAEs) — responsible for connecting members to primary and behavioral health care — can earn financial incentives for showing improvement or hitting targets on certain metrics. Some of these include well child visits, depression screening follow-ups, dental visits, and prenatal care.
Conclusion: On the Horizon
CHI’s Medicaid and Commercial Insurance Access to Care Index offers a high-level view of access by payer across many metrics. It is intended to launch community conversations about access to care and augment ongoing efforts to identify and address challenges.
For example, the Department of Health Care Policy and Financing will release its second Access Monitoring Review Plan (AMRP) in October 2019. This is a federally required report that assesses whether Medicaid member access to covered services is sufficient and comparable with the experience of other people in the same geographic area.
CHI will release findings from the 2019 Colorado Health Access Survey this fall. CHI will continue to monitor access to care and work with stakeholders to understand nuances in how different data sources tell the story of access to care in Colorado.
Methods and Metrics: The Index Explained
The metrics that comprise the Index are divided into three domains: Potential Access; Perceptions and Experiences; and Realized Access. For more information on the methods and data sources, see the Index Methodology.
Potential Access
Potential access examines the building blocks of access to care. It measures whether the infrastructure exists to ensure people can get the care they need. These metrics include the percentage of people with health insurance, the availability of health providers, wait times to see doctors, and whether providers accept certain health plans or new patients.
Perceptions and Experiences
Even when there is sufficient infrastructure to help people get care, obstacles may remain. This domain includes some of the logistical challenges that discourage people from seeing a provider. Some of these barriers are directly connected to the health system or to a doctor’s office, such as whether people felt they were treated respectfully, or whether cost prevented them from getting the care they needed. Other barriers originate outside the medical system, such as a parent skipping an appointment because of difficulty finding child care.
Realized Access
This domain measures whether a person saw a provider and received appropriate care. In other words, it measures how well the Potential Access and Perceptions and Experiences domains have translated into the actual use of health care services. Metrics include rates of access to preventive services and primary care, such as cancer screenings, dental visits, and well-child visits. This domain also measures the percentage of people who did not receive needed mental health services in the past year.
Limitations of the Index
The index is limited to Coloradans ages 0-64. Commercial insurance includes employer-sponsored plans and coverage purchased directly from an insurer, such as through the state’s health insurance marketplace, Connect for Health Colorado.
The health services covered vary for many reasons, such as eligibility characteristics of a Health First Colorado enrollee or the quality of a commercial insurance plan. Although CHI used data on providers accepting Medicaid, CHI did not have information on which providers participated in which commercial insurance networks.
Therefore, counts of providers should be interpreted with caution. Additionally, CHI was unable to adjust for income, health status, and other socioeconomic factors to compare similar populations across payers. As a result, some of the differences in access scores between Medicaid and commercial insurance may be due to these factors.
Full Methods and Sources
Endnotes
1 Colorado Health Access Survey, 2017. https://www.coloradohealthinstitute.org/research/colorado-health-access-survey-2017
2 Colorado Department of Health Care Policy and Financing (2019). FY20 R1 Medical Services Premiums, Exhibit B – Medicaid Caseload.
https://www.colorado.gov/pacific/sites/default/files/3-%20R-1%20MSP%20B.pdf.
3 Specialty care study: Colorado Health Institute (2019). Colorado’s Unmet Demand for Specialty Care. [Insert URL once posted.]
4 Gunja, M.Z., Collins, S.R., Blumenthal, D., Doty, M.M., & Beutel, S. (2017). How Medicaid enrollees fare compared with privately insured and uninsured adults. Retrieved from the Commonwealth Fund website: https://www.commonwealthfund.org/press-release/2017/new-report-medicaid-provides-equal-or-better-quality-health-insurance-coverage
5 The Colorado Health Access Survey, 2017.
6 The Colorado Health Access Survey, 2017.
7 The Colorado Health Access Survey, 2017.
8 Kaiser Health News. (2012). Study: Nearly a third of doctors won’t see new Medicaid patients. Retrieved from https://khn.org/news/third-of-medicaid-doctors-say-no-new-patients/
9 Holgash, K., & Heberlein, M. (2019). Physician acceptance of new Medicaid patients: What matters and what doesn’t. Retrieved from https://www.healthaffairs.org/do/10.1377/hblog20190401.678690/full/
10 The Colorado Department of Health Care Policy and Financing evaluates the sufficiency of Medicaid rates as part of the Medicaid Provider Rate Review process, as required by state statute. See the 2018 and 2019 rate review reports posted here: https://www.colorado.gov/pacific/hcpf/medicaid-provider-rate-review-advisory-committee. Note that behavioral health services were limited to fee-for-service.
11 Colorado Health Institute. (2015). Narrow Networks in Colorado. Retrieved from: https://www.coloradohealthinstitute.org/sites/default/files/migrated/postfiles/Narrow_Networks_in_Colorado.pdf
12 Colorado Department of Regulatory Agencies Division of Insurance 3 CCR 702-4 Series 4-2 https://www.sos.state.co.us/CCR/GenerateRulePdf.do?ruleVersionId=8094&fileName=3%20CCR%20702-4%20Series%204-2 (Page 364)
13 The Colorado Health Access Survey, 2017.
14 Institute for Women’s Policy Research. (2015). Worker’s access to paid sick days in the states. Retrieved from http://www.nationalpartnership.org/our-work/resources/workplace/paid-sick-days/workers-access-to-paid-sick-days-in-the-states.pdf
15 Bureau of Labor Statistics. (2016). Access to paid sick leave, vacations, and holidays varies by wage category. Retrieved from https://www.bls.gov/opub/ted/2016/access-to-paid-sick-leave-vacations-and-holidays-varies-by-wage-category.htm
16 Colorado Health Institute. (2018). Transportation a barrier to care across Colorado. Retrieved from https://www.coloradohealthinstitute.org/sites/default/files/file_attachments/CHAS%20Barriers%20Transportation.pdf
17 Bosselman, A. (2019). Denver’s new bus and train fares are the most expensive in the nation. Retrieved from https://denver.streetsblog.org/2019/01/02/denvers-bus-and-train-fares-now-the-most-expensive-of-major-cities/
18 Coltrain, N. (2018). Colorado’s most vulnerable Medicaid patients say they are left waiting for rides. Retrieved from https://www.coloradoan.com/story/news/2018/02/01/colorados-most-vulnerable-medicaid-patients-say-they-left-waiting-rides/1067659001/
19 Lewis, C., Abrams, M.K., & Seervai, S. (2017). Listening to low-income patients: Obstacles to the care we need, when we need it. Retrieved from https://www.commonwealthfund.org/blog/2017/listening-low-income-patients-obstacles-care-we-need-when-we-need-it
20 Lewis, C., Abrams, M.K., & Seervai, S. (2017). Listening to low-income patients: Obstacles to the care we need, when we need it. Retrieved from https://www.commonwealthfund.org/blog/2017/listening-low-income-patients-obstacles-care-we-need-when-we-need-it
21 The Colorado Health Access Survey, 2017.


 Read the full report
Read the full report
 Download as PDF
Download as PDF