Trouble on the Horizon for Community Health Centers
Federally Qualified Health Centers — commonly known as Community Health Centers, or CHCs — are often considered the backbone of the health care safety net. With support from state and federal grants, these clinics provide much-needed medical care to more than 740,000 vulnerable Coloradans all over the state. This year, for National Health Center Week, CHI is looking at some important developments in the past, present and future of Colorado’s CHCs.
Past: A look back at the Affordable Care Act
When it comes to a potential ACA repeal, the stakes are high for CHCs. The passage of the Affordable Care Act was a pivotal moment for the health care safety net, though the past few months have left many wondering how long President Obama’s signature legislation will last. Although the August congressional recess has given the ACA a reprieve, CHCs remain worried about the potential ramifications of the repeal effort.
In return for meeting certain requirements for access, quality improvement, and services provided, CHCs receive federal grants that other clinics don’t qualify for. They can also receive additional reimbursement for Medicaid and Medicare patients they see.
The ACA took this a step further, and created competitive grants for CHCs to expand their services by opening more clinics, making technological improvements like electronic medical records, hiring and training staff, and various other improvements. This potential for expansion attracted some safety net clinics that were not federally qualified to become CHCs.
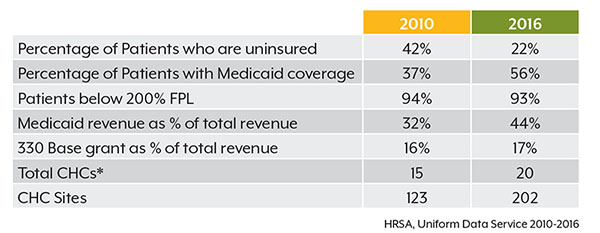
Moreover, Medicaid expansion resulted in a major shift within CHCs. Before the ACA allowed Colorado to offer Medicaid to low-income childless adults, 42 percent of CHC patients didn’t have any kind of insurance. Now, 22 percent of patients are uninsured (see table). This produced more revenue for clinics.
The greatest impact of an ACA repeal would come from proposed changes to Medicaid. CHC patients would theoretically remain protected, because federal law states these clinics must accept patients regardless of insurance coverage. With reduced Medicaid reimbursements, CHCs would have difficulty meeting their costs and keeping their doors open.
Present: On the front lines of Colorado’s opioid crisis
One of the biggest issues facing CHCs across Colorado is the opioid crisis. Across the nation, nearly 12 percent of adults on Medicaid have a substance use disorder. High opioid prescription rates and access to illicit drugs mean that an increasing number of substance use disorders are opiate-related. As the largest payor for behavioral health services in the nation, Medicaid, and the clinics that accept it, have felt the effects of this growing issue.
Thanks in part to the national spotlight placed on the opioid crisis, more support has been made available to CHCs address opioids. Through SAMHSA, ACA, and other federal grants, CHCs are turning the tide on how they approach treating substance use disorder. Colorado Coalition for the Homeless (CCH) recently expanded its integrated services to include MAT treatment, and has been pleased with the outcome. Cathy Alderman from CCH told us that, although implementing MAT would require more of its providers and add another layer of complexity to the system, it quickly became apparent that it was the right move for both the clinic and its patients.
Qualified CHCs have been required to deliver behavioral health services prior to the ACA, but recent state and federal grants have brought these services to more people. For some clinics, this has meant hiring a behavioral health care professional to provide substance use disorder counseling on-site. Other clinics have used grants to train their staff to provide medication-assisted treatment, the most effective approach for opioid abuse.
Future: Challenges on the horizon for CHCs
Community health centers don’t have to look far into the future to find cause for alarm. When asked about challenges facing CHCs in the next five to 10 years, Jennifer Morse from Salud Family Health Centers told us “Honestly, I’m more worried about the next 30 days.” She was referring to the end of September, which marks a major funding cliff for CHCs unless Congress reauthorizes several key programs. Federal grants for CHCs come from discretionary appropriations and the Health Centers Fund, which finances many of the expansion programs made available through the ACA. Without these, CHCs could lose roughly 70 percent of critical federal grant dollars, and many would be forced to shut down. Elected officials on both sides of the aisle have indicated they don’t want this to happen, but the September deadline is fast approaching.
And the CHC grants aren’t the only thing. Funding for the Children’s Health Insurance Program (CHIP) — known as the Child Health Plan Plus (CHP+) in Colorado — expires on September 30. So too does funding for the National Health Service Corps (NHSC), which encourages new physicians to work in CHCs by repaying their student loans. Even under full implementation of that program, many CHCs cite physician shortages as a big obstacle. In mountain communities, where the cost of living is higher than average, the problem is even worse. Clinics find themselves competing against each other for the few providers willing to practice in CHCs.
Time's Up
Though they face significant challenges, Colorado’s community health centers have made significant progress over the past few years by expanding access to care to thousands of Coloradans. Without renewing programs that drove this progress, it will be difficult for CHCs to address future issues like opioids or the physician shortage.
