Colorado Opioid Crisis Response Blueprint
Key Takeaways
- Community leaders and policymakers want to plan now for putting anticipated settlements from opioid lawsuits to the best use.
- Colorado’s opioid experts recommend using the largest portion of the opioid settlement money to expand treatment and recovery efforts, particularly in rural areas.
- All communities are different. While this blueprint provides a guide, investment decisions will need to consider issues ranging from local workforce capacity to sustainable financing.
State leaders have created much of the infrastructure needed to address the problem — including prevention, harm reduction, law enforcement services to address the opioid epidemic, and treatment and recovery supports — but many communities lack the resources to deal with the magnitude of the challenge.
To continue the fight against the opioid crisis, multiple states — including Colorado — sued drug manufacturers and other companies and individuals that contributed to the opioid epidemic. The first settlements in other opioid lawsuits around the country were announced in the spring and fall of 2019. While Colorado’s lawsuit has not settled, there is reason to believe that Colorado could receive settlement funds. Depending on the specifics of the settlements, local communities and/or the Colorado Office of the Attorney General could have a measure of control over how to spend settlement dollars.
It is unlikely that settlement payments, even if large amounts are received, can adequately cover the costs of addressing all the negative impacts of the opioid crisis in communities. Policymakers will have to prioritize how they use the money. This guide can help.
The Colorado Consortium for Prescription Drug Abuse Prevention (Consortium) engaged the Colorado Health Institute (CHI) to help inform a spending strategy for state and local policymakers who are expecting these dollars. In partnership with the Consortium, Colorado Counties Inc., the Colorado Municipal League, the Colorado Medical Society, the Colorado Office of the Attorney General, the Colorado Chapter of the American College of Emergency Physicians, the Colorado Office of Behavioral Health, and other experts, CHI generated a “spending blueprint” on how to best address the opioid crisis. Most items in the blueprint apply just as well to other substances, such as methamphetamines, as they do to opioids.
To make the blueprint, CHI and the Consortium convened a team of experts to identify a list of 20 investment options under four categories: prevention, treatment and recovery, harm reduction, and criminal justice. Experts working in law enforcement, clinical care, prevention, and other areas prioritized these investment options in a survey asking how they would allocate a hypothetical $100 million in opioid settlement dollars.
The results reveal that Colorado’s experts recommend prioritizing treatment and recovery services, followed by prevention, criminal justice, and finally harm reduction. That said, depending on their area of expertise, there was a range of preferences for the best allocation of resources.
This report details the findings of the survey.
What are the Opioid Litigation Settlements?
Colorado’s lawsuit is a Colorado state court case against opioid manufacturers and others. It seeks monetary damages for harm caused to the State of Colorado and its citizens as a result of deceptive marketing of opioids. If there is a settlement of Colorado’s case, funds will be available to address the opioid epidemic.
Separately, the National Prescription Opiate Multidistrict Litigation consists of more than 2,000 federal court cases brought by counties, cities, tribes, and individuals against chain pharmacies and manufacturers and distributors of prescribed opioids. The defendants are accused of exacerbating the opioid crisis by misrepresenting the risks of long-term use of those drugs, aggressively marketing them, and failing to prevent suspicious shipments of prescription opioids. A negotiating class has been formed to provide a method for all counties and municipalities in the United States to join the litigation and receive funds from settlements, as long as at least 75 percent of six different categories of local governments agree to global settlement terms.
Settlement funds received by the state, and separately by Colorado cities and counties, present an opportunity to address the opioid crisis at the local level. While this blueprint provides one guide for communities as they consider strategies to implement locally, other state-level and national resources exist. For example:
- Bringing Science to Bear on Opioids provides an account of current evidence-based approaches to addressing the opioid crisis.
- The President’s Commission on Combatting Addiction and the Opioid Crisis summarizes the results of a federal commission tasked with making recommendations to state and federal policymakers on how to address the addiction crisis.
For Colorado-specific strategies that are aligned with national strategies, see Prescription Drug Abuse Prevention: A Colorado Community Reference.
What is this Guide?
This guide, or “blueprint,” is a tool to help decision-makers at municipal, county, and state levels allocate the opioid settlement dollars received. Other community members — including law enforcement, health care providers, community coalition members, educators, and public health officials — may also use this framework to assess their community’s available resources and gaps in addressing drug abuse and addiction.
Strategies to Address the Opioid Epidemic
The blueprint draws on a survey that asked experts to prioritize 20 potential investments they could make to address the opioid epidemic. The investments are organized into four domains: prevention, treatment and recovery, harm reduction, and criminal justice.
In the survey, Colorado experts were asked how they would allocate a hypothetical $100 million over five years to address the opioid epidemic. Local decision-makers can use this table to apply the same concept to their hypothetical share of a settlement.
Decision-makers can use this tool as they consider what programs already exist in their communities and what gaps remain.
Addressing the Opioid Crisis: Colorado’s Recommended Approach
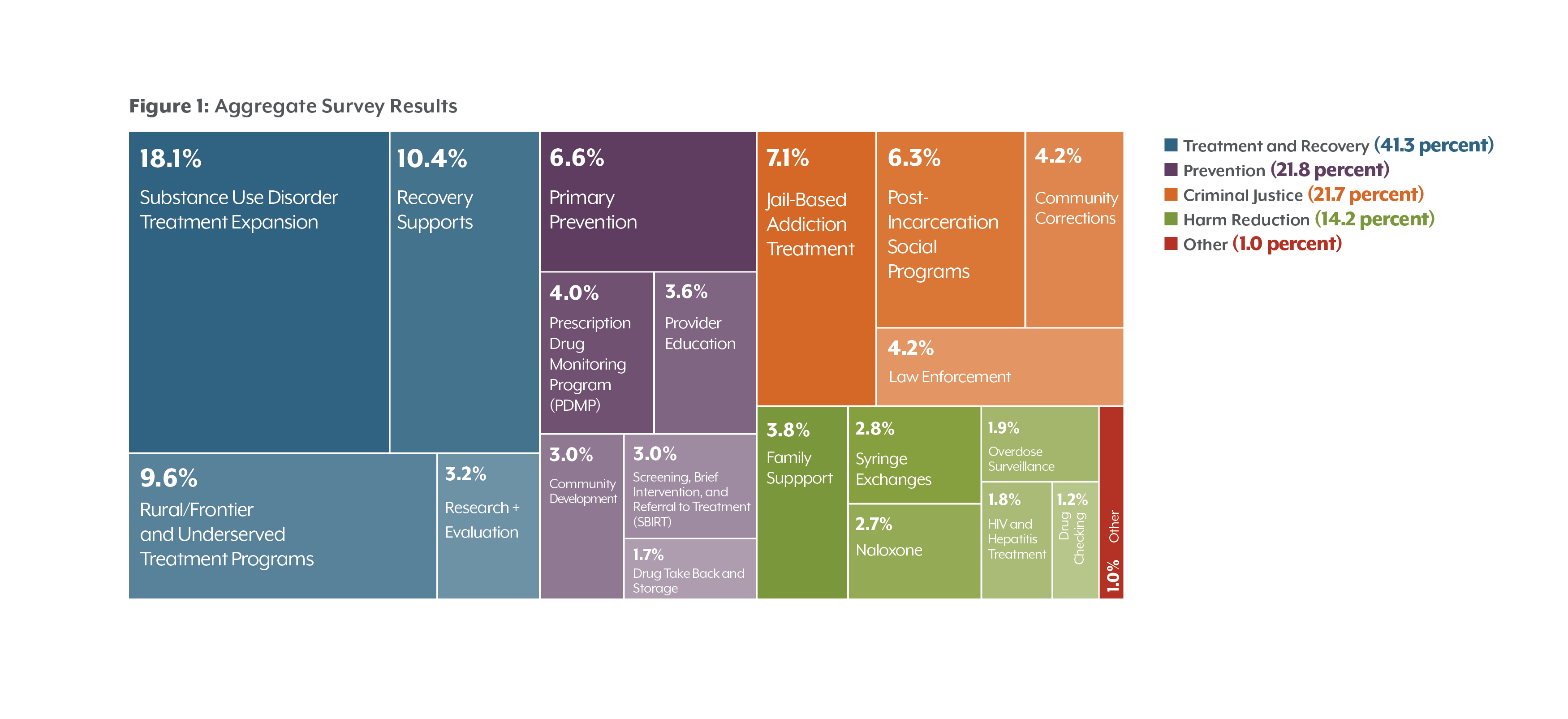
Colorado’s opioid experts identified treatment and recovery (41.3 percent) as the most urgent areas of investment to address the opioid crisis. They devoted less to prevention (21.8 percent) and criminal justice strategies (21.7 percent). Respondents allocated the least amount to harm reduction strategies (14.2 percent).
Although given the option to write in investment suggestions, most experts surveyed did not add to the list — suggesting that this list is a comprehensive view of the options available. Experts allocated only one percent of their potential investment to other strategies not listed below.
Below, the results are illustrated in a series of charts. Each box represents a potential investment area, such as naloxone expansion or primary prevention. The size and color intensity correspond to the share of proposed spending.
There was substantial agreement among the group to allocate the most funding towards treatment and recovery. Within this domain, substance use disorder treatment expansion (18.1 percent) was heavily emphasized, with recovery supports (10.4 percent) and a focus on rural/frontier programs (9.6 percent) almost equally considered as the second priority.
The percentages of funding allocated to the investment domains and items is an average, as experts’ opinions differed in a few of the domains.
Findings by Area of Expertise
To address the unique needs of their community, local decision-makers should consider the priorities and perspectives of different groups of experts. Figure 2 illustrates the blueprint survey results by area of expertise.
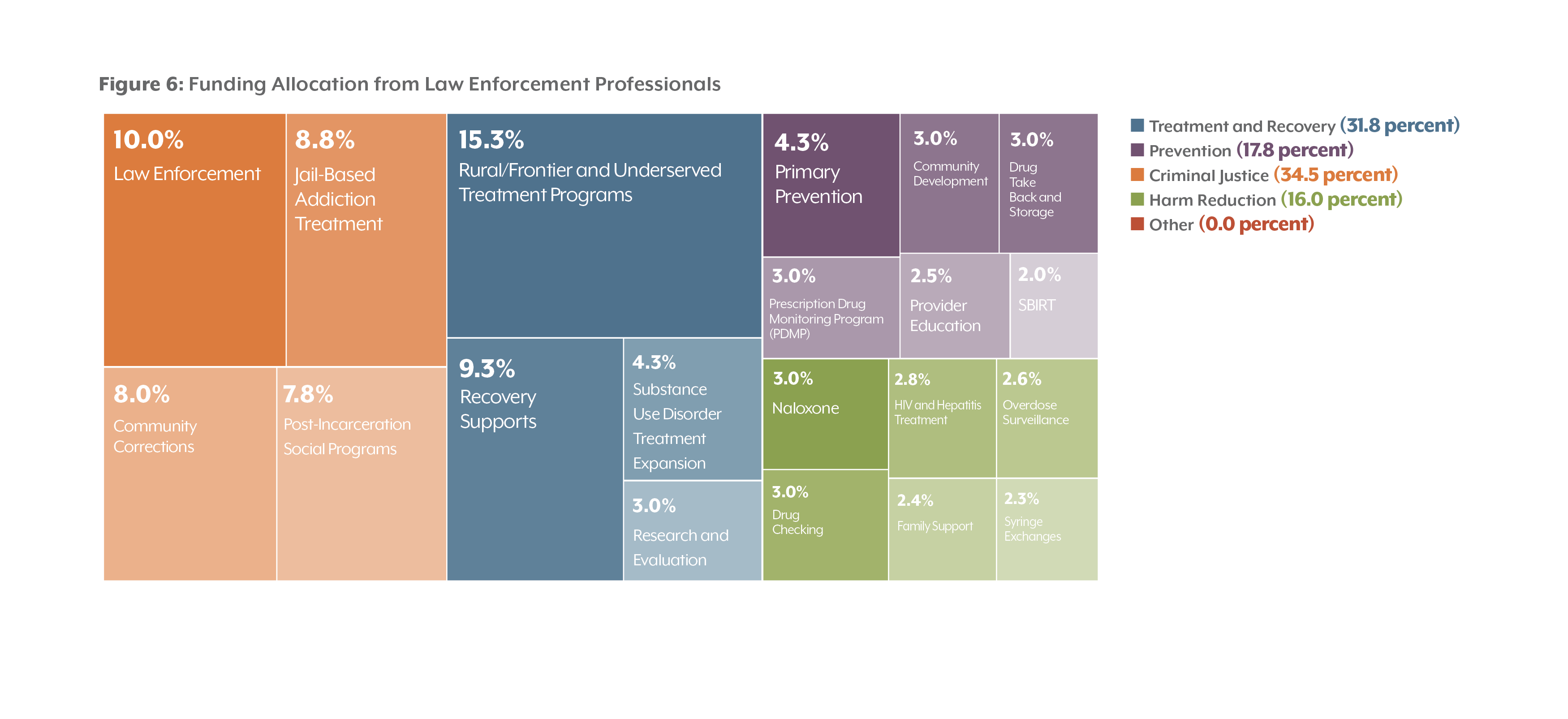
Most groups identified treatment and recovery as their top priority and gave the least allocation to harm reduction. The exception was respondents identifying as law enforcement professionals. Those individuals allocated less funding to treatment and recovery (31.8 percent) than the three other groups and more to criminal justice (34.5 percent).
Two groups ranked prevention as the second highest funding priority, but the other two prioritized criminal justice over prevention.
Harm reduction scored lowest among all groups. Experts may prioritize treatment and recovery over other strategies because those services and supports generally cost more and therefore need additional resources.
On the following pages, four graphics illustrate the results from each of the four expert groups. Though there was agreement across the groups to prioritize treatment and recovery or criminal justice, some groups emphasized different strategies. Those variations are highlighted in each graphic.
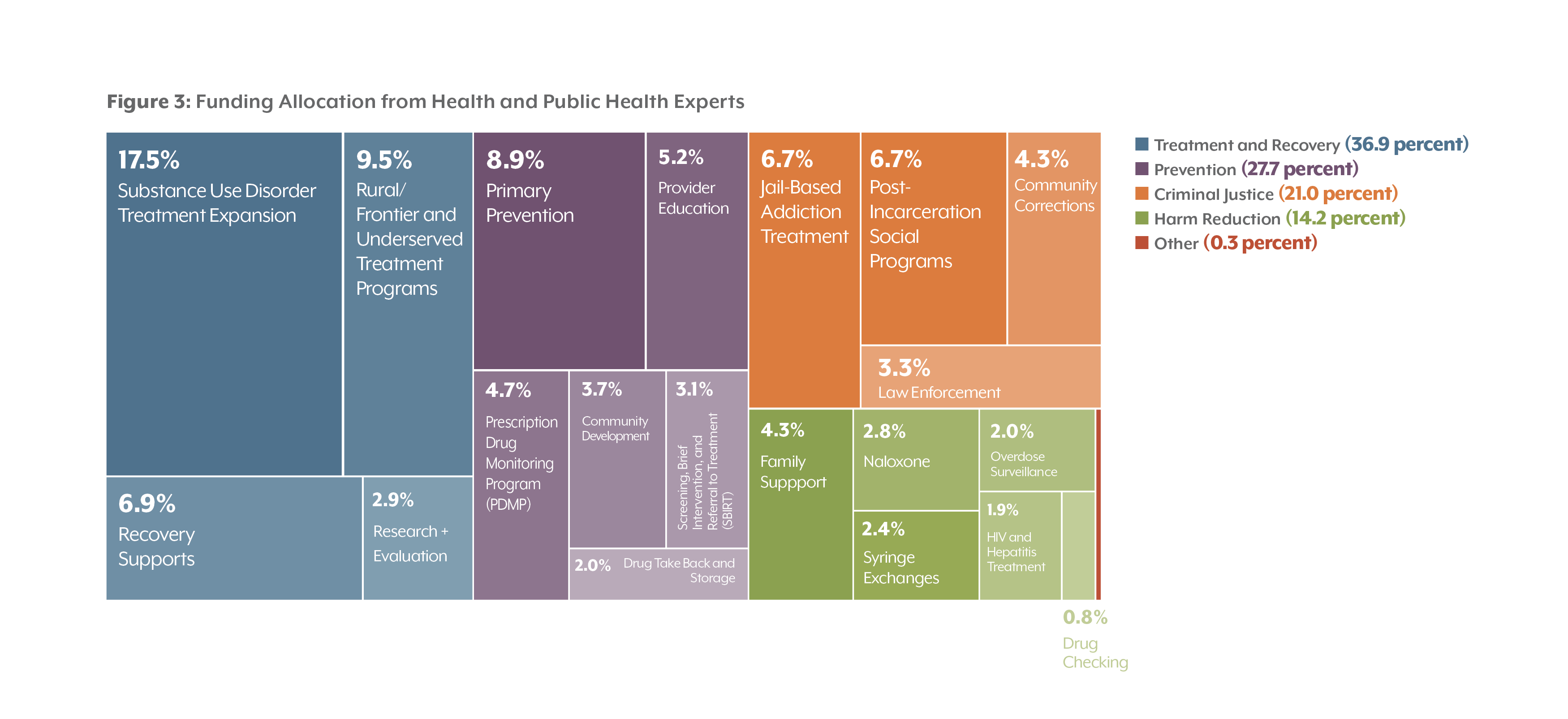
Health and Public Health Experts
CHI found that responses of health care and public health professionals were consistent with those of the overall group. That said, this group recommended investing more in the Prescription Drug Monitoring Program (PDMP) with 4.7 percent of the allocation. They emphasized that linking drug prescribing to electronic health records is critical to addressing the epidemic, and that Colorado is far from having a statewide system in place.
During the Delphi discussion, this group of experts also recommended training allied professionals on reducing access to opioids, such as the investment of funds to promote best practices in opioid prescribing among veterinarians and trainings for employers. In addition, other members of this group recommended training employers on best practices for prevention, including workplace health promotion programs to meet the needs of workers prone to injury and prescription drug use.
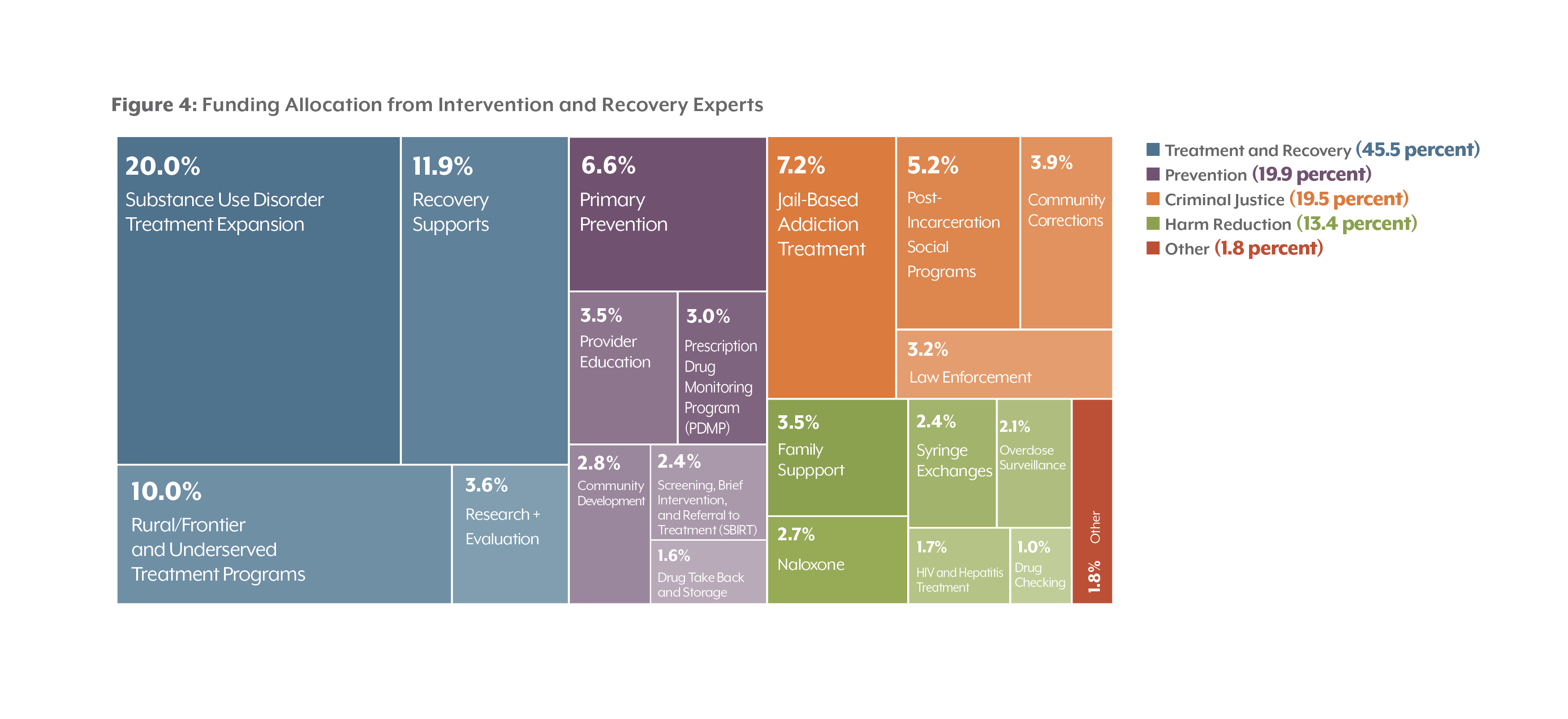
Intervention and Recovery Experts
Intervention and recovery professionals and advocates prioritized treatment and recovery — services that directly affect their work –– with 45.5 percent of the allocation. The group also allocated the least to harm reduction, though they directed as many resources to syringe exchanges (2.4 percent) as most other groups. Meeting participants felt that syringe exchanges were helpful in the downtown areas of large cities but less so in rural areas with sparse populations.
Several respondents wanted to improve the quality of facilities. For instance, one respondent put $14 million toward renovating and purchasing facilities for treatment services. Another respondent recommended $8 million to support those who don’t qualify for Medicaid to obtain treatment and housing assistance.
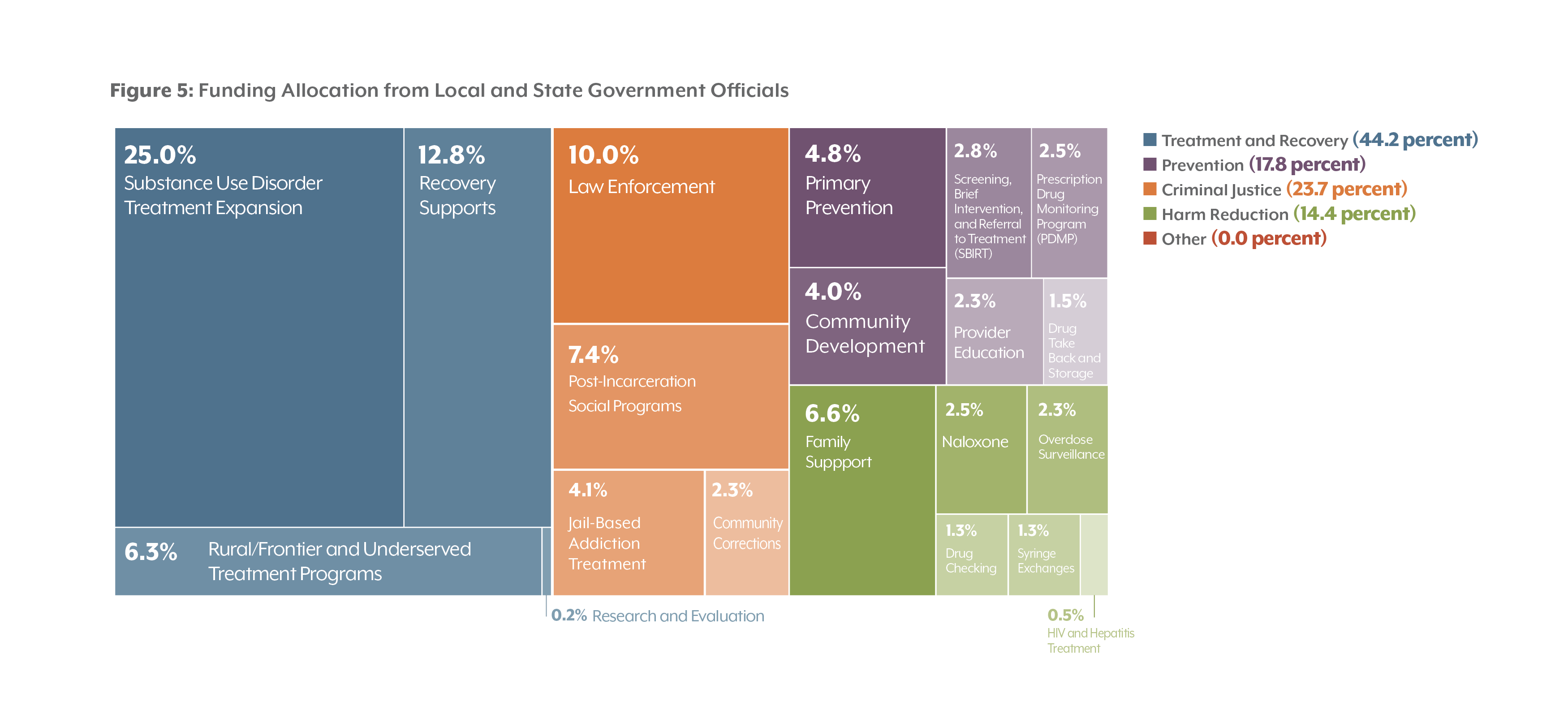
Local and State Government Officials
Compared with other groups, local and state government officials invested more in substance use disorder treatment expansion (25.0 percent). They also recommended investing more in family support (6.6 percent) in the harm reduction domain than any other group. Respondents in this group also allocated significant funding to law enforcement (10.0 percent) — the same amount allocated by law enforcement professionals themselves.
This group also noted several benefits of allocating more dollars toward overdose surveillance. With greater surveillance, policymakers could target areas of need rather than producing a nontargeted response that is less cost-effective.
Law Enforcement Professionals
Law enforcement professionals allocated more funding toward criminal justice (34.5 percent) than other groups. Members of this group also allocated less than a quarter of the amount of funding to substance use disorder treatment expansion compared with other respondents. Other groups devoted around 20 percent of funds to that strategy, while this group allocated 4.3 percent.
Compared with other groups, law enforcement professionals devoted more to rural/frontier and underserved treatment programs (15.3 percent). Meeting participants noted that the group’s strong emphasis on rural/frontier programs was possibly due to the high costs of building the infrastructure in rural and frontier counties to address treatment needs.
Looking Ahead –– Colorado’s Settlements
As state and local decision-makers anticipate potential settlement dollars, they should consider different mechanisms to fund, allocate, and leverage these funds. Several examples are described below:
Competitive funding
Competitive funding is a process of proposal selection based on the evaluation of a team of reviewers.
Noncompetitive funding allocation to communities
In contrast to competitive funding, this form of funding is given to predetermined recipients based on population, the severity of the local drug problem, or other census criteria, as well as government-to-government transfer of funds.
Pay for Success Contracts
These contracts are an innovative approach to improving outcomes and reducing costs to government. A pool of government funds are leveraged to secure upfront capital from private investors to implement services aimed at achieving specific outcomes.
If outcomes are met, investors receive performance-based payments and a portion of savings to government.
Matching Funds
Funds are provided by the government, foundations, or other sources by matching the community contribution to a project. For instance, private foundations could match community settlement funds to leverage and support the blueprint’s strategies.
The Current State of Play
At the time of publication, no opioid settlements have been finalized. It is not known how much money Colorado can expect from opioid settlements or when settlement funds may be received.
Any settlement negotiated by the Colorado Attorney General’s Office will benefit the entire state.
Colorado local governments, cities, and counties can also follow the National Prescription Opiate Litigation known as multidistrict litigation (MDL) 2804.
MDL 2804 includes more than 2,000 lawsuits filed against companies and individuals in the opioid supply chain by counties, cities, tribes, and individuals. If there are settlements in those cases, every municipality, tribe, and county in the United States could receive funds in accordance with an allocation model that accounts for the amount of opioids shipped to the area, the number of opioid deaths in the area, and the number of people in the community who have opioid-related substance abuse disorders.
Information — including an allocation map that estimates how much funding each local government might receive through a settlement of MDL cases — is available at the MDL 2804 negotiation class website: www.opioidsnegotiationclass.info.
Another development to follow is the Purdue Pharma bankruptcy case that is ongoing in bankruptcy court in New York. Purdue Pharma has proposed a structure to resolve lawsuits against it that could result in distribution of funds.
Policy Considerations
This blueprint provides a guide for local and state decision-makers as they allocate resources to address the opioid crisis and other behavioral health challenges. However, depending on individual community needs — from workforce shortages to existing financing streams — community leaders should adjust their allocation. Several considerations are described below:
Breadth versus depth. Some communities may benefit from broad financial support across their behavioral health system. But others may create the biggest impact from a significant influx of funding into one part of the system — such as building a system of recovery supports or increasing the number of medication-assisted treatment providers in the region. What impact could a community create by focusing investments in one domain?
Outcome alignment. Policymakers should identify key outcomes to target — and in what time frame — and prioritize their investments accordingly. For example, if the goal is to reduce misuse of all substances and not just opioids, then policymakers could focus on family supports, access to health care, and primary prevention. But if the goal is to reduce the number of opioid-related deaths, then investing in treatment and overdose prevention would be a higher priority.
Cost-effectiveness. This blueprint offers a general guide for policymakers considering how to use opioid settlement dollars. But it does not quantify the needs for each item in the survey. For instance, if $20 million were allocated to treatment, how many additional people could be served, and how does that match up with the need? Policymakers will need more information before they can understand exactly what they can “buy” with their share of the settlement.
Sustainability. When thinking long-term, policymakers and communities should consider the sustainability of the investments and grant funding, as well as strategies themselves. If the time line for the goal is shorter, policymakers should take into account the threshold at which program funding can adequately address the issues within the allotted time frame.
Spending capacity. Following an analysis of a community’s resources, policymakers should think about the extent to which these service areas have capacity to spend the dollars. For example, can treatment centers hire and pay more staff? What is the cost of training new staff or relocating them to certain areas of need?
Though this analysis recommends focusing potential opioid settlement resources in Colorado on treatment and recovery, other recent analyses have taken different approaches. For example, other researchers published in the Milbank Quarterly recommended devoting most resources to a national organization — similar to the Ryan White HIV/AIDS program — that would in turn make grants to needy communities.
Conclusion
As of December 2019, Colorado communities are waiting on whether settlements will come out of the multiple ongoing opioid lawsuits. It is not clear how large settlements will be, how settlement funds will be allocated, or when settlement payments will be received. This analysis provides guidance to local and state decision-makers in communities considering how to allocate these resources — and how to strengthen their service systems in response to the opioid crisis.