Methods
The Colorado Health Institute (CHI) built a mathematical model to project the effects of the Medicaid reforms in the American Health Care Act (AHCA) proposal on Colorado’s state budget and Medicaid enrollment through the year 2030.
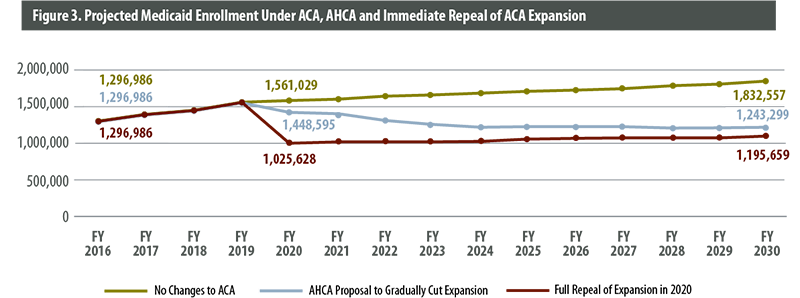
1. Enrollment Projections
We began with public data from the Department of Health Care Policy and Financing (HCPF) that shows fiscal year (FY) 2016 Medicaid enrollment. Membership in Medicaid has grown rapidly since Colorado expanded eligibility in 2014, which makes it difficult to project future enrollment based on past trends. However, growth in enrollment has slowed recently. CHI projected that the expansion and non-expansion Medicaid enrollment would both continue to slow at their current rates until they reach the level of population growth. At this point, we project that Medicaid non-expansion enrollment will grow at the same rate as the Colorado population and that Medicaid expansion enrollment will grow at the rate of the Colorado adult population. We extended these projections to 2030, when we project that Medicaid enrollment would reach 1,832,557 under the current system.
This method allowed us to project the growth of different segments of the Medicaid population — children, seniors (those dually eligible for Medicare and Medicaid), adults who qualified for Medicaid before the ACA and adults who qualified after the ACA. Some of these groups get a 50/50 match from the federal government, while people in the ACA expansion bring enhanced funding of 90 percent or more from the federal government.
2. AHCA Enrollment Restrictions
Starting in 2020, the AHCA ends enhanced federal matching funding for people who gained Medicaid membership under the ACA expansion but become ineligible for 30 days or more. CHI used Colorado’s FY 2016 “churn” rate — the percentage of people who become temporarily ineligible for Medicaid during a given year —to project the effects of the AHCA. In FY 2016, 21 percent of the Medicaid population churned out of the program. We applied the 21 percent rate to the projected Medicaid population in 2020 and compounded it annually to project a Medicaid population of 1,243,299 in 2030. That is nearly 600,000 fewer enrollees than it would have been under the ACA. This projection assumes that Colorado would choose to cut its Medicaid eligibility for people who lose the ACA’s enhanced federal match.
We calculated a third scenario. Assuming that Colorado decides to cut Medicaid eligibility for all ACA expansion enrollees — including those who would retain the enhanced federal match under the AHCA —an additional 47,640 people lose Medicaid coverage in 2030. Under this scenario, we project the lowest 2030 Medicaid enrollment: 1,195,659.
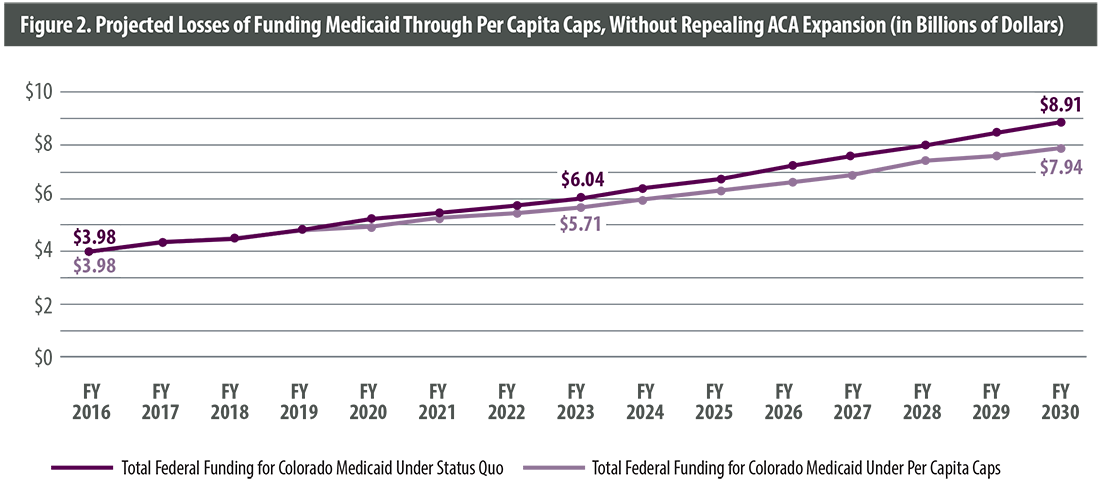
3. Per Capita Growth Rates
CHI then projected Colorado’s Medicaid spending under both the current system and the AHCA. To project current spending, we used data from the Kaiser Family Foundation on the growth in per person spending in Colorado’s Medicaid program by type of enrollee from FY 2000 to FY 2011, the most recent years available. We extrapolated this figure out to 2030.
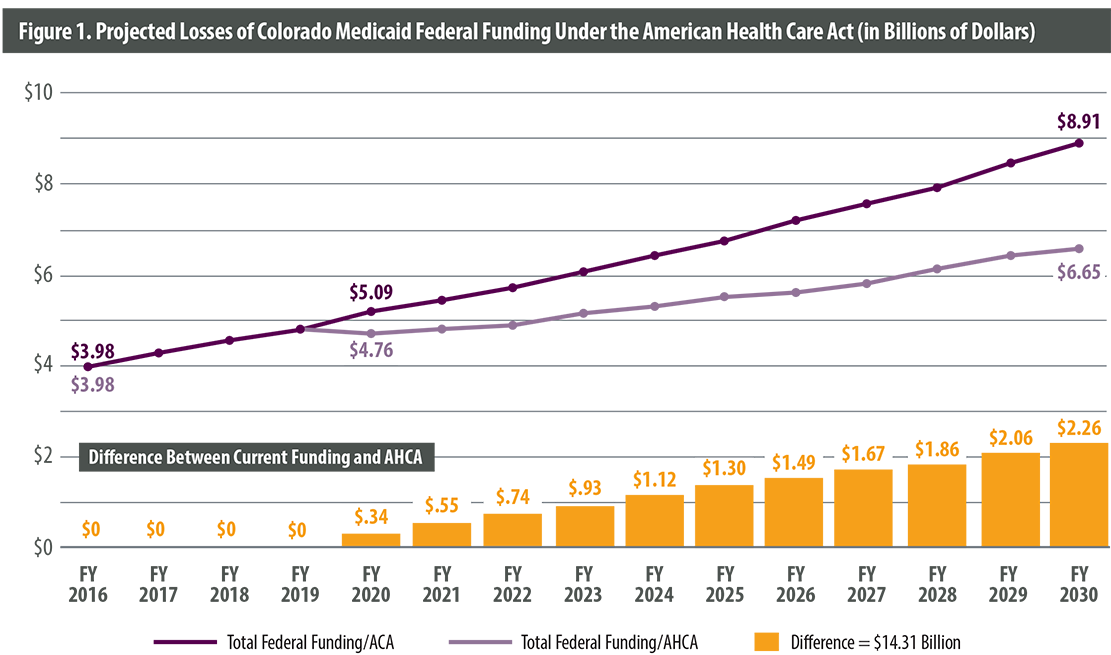
The AHCA would change federal funding for Medicaid to a per capita allotment system. To project spending under this system, we used the formula specified in the AHCA, which considers Medicaid enrollment growth plus the medical care component of the Consumer Price Index (CPI) — the U.S. Department of Labor’s official calculation of inflation. To project medical care CPI, we calculated the compound annual growth rate of medical care inflation from September 2007 to September 2016 and extrapolated this figure out to 2030.
4. Per Capita Federal Spending
We calculated per person federal spending by first determining total medical and behavioral health expenditures by Medicaid group – non-expansion adults, children, seniors and expansion adults – in FY 2016 based on public HCPF data.
Growth rates calculated in Step 3 were applied to this amount to estimate per person spending through 2030.
Finally, we adjusted our projections of Medicaid enrollment by group, separating those that would receive less funding due to the restrictions on the enhanced federal match for new Medicaid expansion enrollees. We calculated federal spending for each enrollment group, taking into account that fewer people would qualify for the enhanced federal match provided by the ACA.